Recently Paul Saladino, a psychiatrist, and proponent of the carnivore Diet appeared on Joe Rogan’s podcast. I have previously debated Saladino and found that he liked to cherry-pick his evidence, focus on weak mechanistic data, and ignore large volumes of evidence counter to his bias. As soon as this podcast went up, my inbox piled up with requests to debunk his talking points. Now, I don’t like to analyze something to debunk it because that is biased in and of itself. So I tried to give the podcast a real chance to present evidence and critically evaluate it. After finishing this article, I can say that it was worse than I ever could have imagined. It was far worse than The Game Changers. There were so many insane claims that it took me far longer to finish this article than it did any of my previous critical analyses of films or appearances on Rogan’s podcast (i.e., Wilks, Kresser, Taubes, Guyenet). I am not expecting this article will change the minds of any hardcore Carnivore diet advocates. Still, for the average person just looking for the truth and confused by all the different diets out there, I hope this can help bring some clarity…and sanity to the discussion.
Also, special thanks to Kevin Bass for his contributions to this article, most notably addressing the first few claims regarding plants being “toxic” as well as many of the claims regarding ancestral nutritional intake.
And without further ado, let’s descend into madness.
Quick Access Table of Contents:
- Plants are toxic (00:41 – 10:08)
- Plants aren’t even good for us (14:12 – 21:37)
- Meat is a superfood (25:00 – 29:00)
- Farming practices (34:18 – 35:50)
- Intermittent fasting (46:10 – 47:35)
- Carnivore for autoimmune issues (57:00)
- Claims about hunter-gatherer tribes (1:03:03-1:10:42)
- Claim about Paul’s liver supplements (1:32:40)
- Claims about saturated fat, PUFAs, LDL, and cardiovascular disease (1:40:10 – 2:01:55)
- Claims about dietary fiber (2:14:57 – 2:17:41)
- For heart health ‘eat like the Hadza’ quote (2:21:57)
- Vegan Diets (2:24:00)
- Grass fed beef vs grain fed beef (2:49:20)
- If you eat a lot of meat, you don’t need to supplement creatine (2:54:41)
- Final claim about plants (3:00:30)

00:00:41 Claim: Joe says that most plants are inedible, but almost all animals are edible. Therefore, he concludes that eating “mostly meat” makes sense.
Reality: The argument that plants are less frequently edible than animals, and therefore humans should consume an “animal-based diet” is specious. You can see this by looking at the implication of the argument: should all animals consume an animal-based diet because “all animals are edible, while only some plants are”? No, because feeding an animal-based diet to many herbivores will cause their malnutrition and death. Therefore, the fact that all animals are edible while most plants are not says nothing about whether any given species should eat or is “designed” to eat an “animal-based diet.” This includes humans.
If this argument meant humans should eat an animal-based diet, it would also mean that all herbivores should also eat such a diet, and we would recommend that all pet turtles, rabbits, and hamsters also consume an animal-based diet. Remember those gorillas eating pounds upon pounds of vegetables from my Game Changers rebuttal? They would also have to consume animals. If they did so, it would quickly lead to the deaths of all of our pets. A pity. It follows that we must determine what the optimal human diet should be from other scientific data. It also follows that knowing “all animals are edible while most plants are not” is a useless syllogism in figuring out the optimal diet for a human or any other animal.
00:04:19 Claim: Plants make defense chemicals known as phytoalexins. These compounds are toxic. Therefore we should eat an animal-based diet.
Reality: According to this argument, because plants might produce “toxins” that provide defense against predation, we should eat animals and not plants to avoid these toxins. The problem with this argument is similar to the previous; does this mean all herbivores should become carnivores? No, because many herbivores would die on a carnivorous diet. It follows that you can’t determine an optimal diet by the fact that plants have defense chemicals or not. Through scientific observation, however, you can discern the kind of diet on which each species best thrives.
Note that while many plant compounds are “toxic,” many compounds in meat are also toxic, especially to herbivores. For example, a dog can eat a lot of cholesterol without ill effect. Rabbits, on the other hand, will rapidly develop heart disease when fed even modest quantities of cholesterol. This is because the compounds in meat are as disruptive to biological homeostasis as the compounds in any other food. Consider that feeding a 40 or 50lb dog a pound of meat represents a larger percentage of body weight in terms of muscle suddenly being added to the biological system of the dog. The dog has the machinery to quickly consolidate and metabolize this new mass of protein, hemoglobin, iron, cholesterol, and countless other compounds concentrated in meat. The rabbit, consuming a similarly large proportion relative to its body weight, does not have this metabolic machinery. What this means is that an animal can be “poisoned” not just by plant defense chemicals but by the intrinsic metabolic composition of the food item itself if the animal is not adapted to consuming that particular food.
Therefore, as we saw above, one cannot conclude the presence of defense chemicals in plants, whether animals or plants are more appropriate to any given species. This must be determined empirically, i.e., from actual scientific data. Using the best techniques available, we must study whether plants or animals are nutritionally suitable for the optimal health of each species. If we are going to be fair, there are quite a bit of mechanistic data for specific components of meat to be carcinogenic/atherosclerotic such as TMAO, heterocyclic amines, and heme iron. [1][2][3] I’m not saying this means meat causes cancer. I think the data is not well elucidated and semi-weak because it relies almost exclusively on tenuous mechanistic data linked with conflicting epidemiological data. However, Paul is using that same logic to argue that plants are toxic. As we will see moving forward, Paul has a pattern of invoking a specific logic when it fits his bias and discarding it when it does not. This is the first many examples of that.
Finally, when it comes to “toxic” compounds, the dosage makes the poison. If plants were so toxic, then why in the world do some of the longest living people in the world tend to eat mostly plant-based diets? [4][5] If plants are trying to kill us through toxins as a defense mechanism, they are doing a shitty job of it so far. And the phytoalexins Paul mentions as toxins? I can’t find any evidence that they lead to adverse human health outcomes, but there is evidence they have anti-tumorigenic effects. [6] I guess Paul left that part out.

00:04:35 Claim: “What if these plant chemicals are not good for us? [They]… affect thyroid, androgens, sex hormones, make you have diarrhea, nausea, or kill you.”
Reality: That which can be asserted without evidence can be dismissed without evidence. Where is the evidence that these plant compounds can kill you? Where is the evidence that they affect the thyroid? Yes, you can find individual compounds in plants that, when isolated in high doses, may affect the thyroid. An examination of the literature on actual whole food plant consumption shows that people who suffer from thyroiditis may consume fewer plants and more animal fat. [7] As far as them affecting your sex hormones, I can only imagine he’s referring to soy phytoestrogens. There is evidence that these phytoestrogens do have biological activity, but this includes both positive and negative effects. [8] Whether or not these compounds are positive or negative for health likely depends upon the dosage and the individual. That said, there’s little evidence eating soy will reduce your testosterone.[9][10]
00:06:05 Claim: Environmental hormesis and molecular hormesis are different things, i.e., we somehow get benefits from the stresses of cold, heat, ketosis, exercise, etc., but we get no such benefits from plant compounds because plant compounds have side effects (such as on the “thyroid, androgens, sex hormones, make you have diarrhea, nausea, or kill you [00:04:35]).
Reality: Saladino suggests that plant compounds are not healthy because while they increase the body’s defenses against oxidative stress—which is associated with aging—they also produce “off-target effects,” which are toxic to the organism. He calls this “molecular hormesis,” a pseudoscientific expression that he “came up with” while writing his best-selling diet book. In contrast, “exercise, ketosis, sunlight, sauna”—which he calls environmental hormesis, another pseudoscientific term—does not produce such off-target effects.
This is a false dichotomy. Exercise, for example, is known to produce both acute and chronic disruptions in thyroid, androgen, and sex hormone production. Saladino alleges these disruptions are an “off-target” characteristic only of plant compounds.[11][12][13][14] Exercise can also cause diarrhea, nausea, and, like plant compounds, even “kill you.” [15][16][17] Moreover, aerobic exercise, like the plant compounds that he inveighs against later in the interview, also causes acute DNA damage, as can sunlight and sauna.[18][19][20] (It is questionable whether ketosis is a hormetic stressor like exercise, sunlight, sauna, and plant compounds.) There are also a range of other “off-target” potentially harmful effects for all of these approaches, including an increase in acute inflammatory and oxidative stress markers, acute hypertension during resistance training, elevated stress hormone and suppressed immune function, and even heart attack, stroke, and atrial fibrillation in the case of exercise and sauna. [21][22][23][24][25][26][27][28] As you can see, by cherry-picking case studies and individual mechanisms, I can even make exercise sound scary.
Given that the changes in biomarkers from exercise, sunlight, and sauna are often quite similar or even worse to those that are called “dangerous” from plant molecules, this dichotomy between molecular and environmental hormesis proposed by Saladino is unfounded, which is not surprising since he invented it without credible formal training in nutrition to market a popular diet book.
Interestingly, Paul discusses how great exercise, sun, and sauna are because they turn on our natural antioxidant systems like Nrf-2 (8:24). Paul conveniently leaves out the fact that there’s evidence several plant foods also activate Nrf-2.[29][30][31][32] Either Paul doesn’t know this, omits it purposefully, or is somehow claiming that the Nrf-2 activation from exercise, sauna, and sunlight is somehow different from the Nrf-2 activation from these plants.
Paul’s discussion about the “side effects” of plants is so disingenuous considering his position regarding meat intake. Red meat, in particular, has been demonstrated to increase oxidative stress, inflammation, and a whole host of other things Paul claims plant foods do, including a red meat derived glycan that promotes inflammation and cancer.[33][34] I’m not saying red meat causes cancer; what I’m saying is that I can find compounds in red meat that do the same things that Paul is claiming, yet there is no discussion of these compounds because Paul is cherry-picking.
00:10:08 Claim: Sulforaphane is very clearly a toxin
Reality: It’s so toxic that it protects against cardiovascular disease, neurodegeneration, and cancer. [35][36][37][38] Boy, those plants keep making these “toxic” compounds that seem to have the side effect of helping us not die. Paul keeps using this word “toxic,” I wonder if he’s aware of its actual definition.
Paul goes on to state that sulforaphane can be beneficial, but it also has side effects. You mean just like heme iron, Paul? [39][40][41] Heme iron can be beneficial and also have possible adverse effects in too high of a dose. I am a fan of protein, and I eat meat. That said, it’s disingenuous to point out that there are compounds in plants that can have side effects (if you take in ridiculously high doses) when there are compounds in meat that do the same damned things.
00:14:12 Claim: There are studies comparing low, medium, and high intake of vegetables and 4,8, and 12 weeks and they show no difference in inflammatory markers, oxidative stress markers, and DNA damage.
Reality: Paul is likely referring to a 12-week study in people with COPD where there was no effect on markers of inflammation and oxidative stress. [42] As per his M.O., however, he is cherry-picking and neglecting other randomized controlled trials and meta-analyses that did show an effect of fruits and vegetable intake on oxidative stress and inflammation. [43][44][45] The authors of a meta-analysis on fruit and vegetable intake on the discussed parameters stated “the majority of the intervention studies (68%, n = 48) reported beneficial effects of fruit or vegetable intake on ≥1 biomarker of systemic or airway inflammation. A meta-analysis of included studies showed that fruit or vegetable intake decreased circulating levels of C-reactive protein and tumor necrosis factor-α (P
00:15:32 Claim: There are no nutrients in plants that you can’t get in equivalent or more bioavailable forms from meat.
Reality: What about all the compounds he just claimed were toxic? Are they in meat too?
00:17:15 Claim: “10mg of vitamin C is all that’s needed to prevent scurvy.” Joe responds that 10mg still isn’t an optimal level for health, to which Paul says that we don’t know.
Reality: We don’t precisely know, sure, but we don’t exactly know a lot of stuff, but we have a pretty damned good idea as we know that neutrophils (immune cells) will reach about 80% saturation at about 75-100mg of vitamin C intake. [46][47] This is an example of Paul doing a bait and switch. He’s trying to de-emphasize the importance of vitamin C because he knows animals aren’t a good source of it by saying you can prevent scurvy with just 10mg per day. Yes, you can avoid scurvy with 10mg of vitamin C per day, just like you can avoid protein deficiency at 50g intake per day. That doesn’t say anything about what is optimal for health.
00:20:06 Claim: Paul cites a meta-analysis about how there is no effect of vitamin C on the common cold.
Reality: I mostly agree with Paul. I just want to point out that he is citing a meta-analysis here, which in previous debates he had dismissed when they did not fit his bias. Another example of Paul using a specific logic or method of research when it suits his bias, then discarding it when it does. That said, vitamin C does very little to prevent the common cold but may reduce cold duration and severity. [48][49][50] FYI I included another meta-analysis in my citation [50].
00:20:37 Claim: Epidemiology is misleading
Reality: Epidemiology (correlation studies) have distinct limitations and cannot be used to infer causation. HOWEVER, I am pointing out Paul’s statement here because, as we will see later on, Paul is happy to cite epidemiological studies when they support his bias but discard them when they do not.
00:21:37 Claim: If you have metabolic dysfunction (nebulous term), it will lower vitamin C levels.
Reality: The implication here is that you can’t infer that low vitamin C is causing health problems because it could be the reverse; these health problems cause a decrease in vitamin C levels. Yea, it could be. But this is another example of Paul being a hypocrite. Paul has been a big advocate for not dropping LDL cholesterol because, during infection, we see reduced LDL levels (more on this later). [51] This is the EXACT. SAME. THING. He doesn’t want us to infer that reduced vitamin C causes health problems, but rather health problems cause low vitamin C, but in the case of LDL, he completely flip flops his argument. Just another example of Paul using one type of logic, then discarding it when it no longer fits his bias.
00:25:00 Claim: Long ramble about how you should eat an entire animal, not just the meat
Reality: Paul uses many stories and studies of old tribes that would eat all parts of the animals and uses this to imply that this means those particular parts must be healthy for us. The reality is that they ate all these things because they could not afford to NOT eat all of the animal because it’s stupid to waste any part of an animal when you don’t know how long it will be until you’d get another kill.
00:29:00 No Claim: I just want to point out that Paul walks around with raw liver in his bag. Alright then, moving on.
00:34:18 Claim: Factory farming is terrible, and there are many corn and grain subsidies that support it.
Reality: While corn and grain subsidies DO support factory farming, so do animal subsidies backed by the animal industry. This is another example of Paul cherry-picking his information based on what fits his bias as the estimation is approximately $283 million in government subsidies go to animal production. [52][53][54] While the lobbying crop production was greater than animal (23 million vs. 12 million), the fact remains that the US government spends plenty of money subsidizing animal production. Further, this demonization of factory farming is interesting, considering Paul thinks the Carnivore Diet is optimal for health and wants to get as many people eating this way as possible. What kind of farming does he believe will support this type of demand? Local farmers? Unlikely. The fact is, the very thing he’s pushing for would increase the demand for the factory farming practices that he is so willing to demonize. [55][56] To be clear, we aren’t advocating for factory farming. It certainly has issues, but Paul’s willingness to demonize it simply highlights his cherry-picking of facts and inclination to use a certain logic when it suits his bias, but then discard that logic when it doesn’t.
00:35:50 Claim: 85% of a cow’s life is eating grass even if they are grain-finished. The implication being that it’s very sustainable to have cows exclusively grass-fed.
Reality: This ignores herd dynamics. Mathematical modeling of a shift to exclusively grass-fed beef would require increasing the national cattle population by ~30%. The current pastureland resource can only support 27% of the current beef supply (27 million). [57] Indeed, these authors concluded that “an entire grass-and forage-raised beef scenario can only be met domestically if beef consumption is reduced, due to higher prices or other factors.” If carnivore is the way to optimal health (the evidence suggests it’s not but let’s play this game for a moment), then switching to exclusively grass-fed beef will have FEWER people eating beef, not more.

They follow up with a discussion about how beneficial it is for animals to live on land, and their habitation is healthy for the land. Paul uses the example of how nutrient-rich the soil was in the middle of the country when herds of millions of bison roamed. One problem with this is we aren’t talking about herds of a few million. We are talking about 100 million. You can’t underestimate those ecological ramifications. Paul discusses how great the ecosystem is when animals live on the land, but an ecosystem exists in a delicate balance. Overpopulation of any one species can decimate an ecosystem. Conventional farming beats grass-fed farming in terms of the carbon footprint, as it requires fewer animals, land, water, and fossil fuels to produce the same quantity of beef. [58] To be fair, there is an argument made that with grass-fed, you have more significant sequestration of carbon, so even though there is greater CO2 production, more of it may be sequestered with grass-fed farming. [59] It certainly is not as clear cut as Paul is making it out to be, and of course, he is not presenting any of the opposing data which doesn’t support his agenda.
00:46:10 Claim: Joe mentions a recent study that showed that intermittent fasting had no weight loss benefit. Paul says the “devil is in the details” and starts down the rabbit hole of asking, “How were they intermittent fasting” and “Were they using junk food?” and “What kind of oils were in their food?”
Reality: This demonstrates a blatant misunderstanding not only of this study (we will get into that soon) but of randomized controlled trials and what “randomization” means. It is easy to criticize a study when you have not read it, but the point of a randomized study is to eliminate bias between subjects. Let’s say you wanted to study intermittent fasting. Let’s also say you didn’t randomize properly, and you said people could choose to do the intermittent fasting group or the continuous meal group. Perhaps people who are more inclined to eat junk food might pick one group vs. the other. This is why groups are RANDOMIZED during a controlled study. Sure, some may be more inclined to consume junk food, but it’s improbable that the intermittent fasting group happened to get all the fast-food junkies when randomized.
Now, let’s discuss the study. “Who would do a study like that?” Joe asks. The study he’s referring to was done by a researcher named Ethan Weiss, who lost weight on an IF approach and believed that this study would show that IF was superior to continuous feeding. [60] When it comes to study design, it’s easy to critique limitations, but we have to understand that it all depends on what you want to test. Dr. Weiss found it easy to lose weight on an IF approach and decided to compare a continuous meal (CMT) approach where people had to consume at least three meals per day spread out vs. eating all their food in eight hours. The groups would be given no instructions on how many calories to consume because the researchers wanted to see if IF was superior for satiety and for spontaneously reducing calorie intake. [61]
The study was 12 weeks in duration, and they found no differences in weight loss between the two groups. They also found there was no difference in cardiometabolic benefits between the groups. The IF group did lose a more significant amount of appendicular lean body mass than the CMT group, but it’s difficult to know if that’s an IF effect since we don’t know if the protein intakes between the two groups were different, and protein is essential for maintaining lean body mass. So, we are left to speculate. It’s easy to highlight this limitation but remember the researchers were trying to answer whether or not employing an IF approach would spontaneously cause weight loss. The subjects did lose weight. They just did not lose more weight than those in the CMT group. This is consistent with a recent meta-analysis examining IF vs. continuous meal feeding approaches, demonstrating that weight loss is no different when calories are equated between groups. [62]
Sadly, news media outlets sensationalized the results to read “Time-Restricted Eating Doesn’t Work for Weight Loss.” [63] That is simply not true and is not what Dr. Weiss’ study found. IF did have a benefit for weight loss; it just wasn’t superior compared to the CMT group. This is a PERVASIVE misunderstanding throughout nutritional debates in the Twitterspace. We might say something like “a ketogenic diet has no metabolic advantage for weight loss.” What people hear is “the ketogenic diet doesn’t work.” Typically, what they respond with is “that’s BS, I lost X number of pounds using a ketogenic (or any other dietary approach being discussed) diet!”
The point is ANY diet can work for weight loss if it allows you to achieve a sustained calorie deficit. To date, no specific diet has shown superiority for weight loss when calories and protein are equated. Further, no diet has emerged as superior for promoting adherence. [64][65] Therefore, whatever the INDIVIDUAL finds easiest to adhere to in the long term will likely produce the best results for that particular person. This seems dependent on the individual’s preferences, lifestyle, and psychology. All that said, if someone PREFERS intermittent fasting, they most certainly can lose weight on it, but it does not appear to be physiologically superior for fat loss. There is some concern regarding it not being optimal for lean body mass, but more research is needed. Paul’s criticisms show little understanding of how research works, specifically randomized controlled trials.
00:47:35 Claim: When you exhaust the glycogen in your liver, you turn on autophagy (speaking about intermittent fasting).
Reality: Autophagy is not something unique to intermittent fasting, although people have tried to make it appear that way. Autophagy is not something that turns “on” or “off.” Autophagy is an important and continually occurring cellular process. The question is whether or not the relative rates increase or decrease. Yes, fasting can increase autophagy. So does regular old caloric restriction where you don’t intentionally fast. [66][67][68] A direct quote from a research paper examining the literature on autophagy stated
“CR (caloric restriction) represents the most robust non-genetic autophagic inducer” and concluded that “modulated autophagy can be achieved by both fasting and CR, and plays a crucial role in normal function and hemostasis of cells.” [69]
Can increasing autophagy have benefits? Yes. But at this point, those benefits do not appear to be unique to fasting and can be achieved through a normal calorie deficit. There is no evidence we are aware of that indicates liver glycogen needs to be depleted to increase autophagy, nor do ketones need to be present for autophagy to increase.
Furthermore, so many people like to make these processes out to be black or what, good or bad, but physiology doesn’t work that way. Autophagy is a big buzzword right now, but too much autophagy is a BAD THING and can cause cell death or apoptosis. And autophagy is part of the degratory pathway of the cell and acts in opposition to anabolic pathways. Many people claim IF is also optimal for anabolism while also touting the benefits of autophagy, but these two processes are in opposition. If something increases autophagy, it is unlikely that it will also be optimal for anabolism.
00:51:15 Claim: Joe says fruit was only available during part of the year, but animals were available year-round to our ancestors to eat.
Reality: It would likely depend on the specific tribe and location. While there is evidence that hunter-gatherers obtained a large amount of their energy from animals, it varied based on food availability. [70][71] Food availability differed HIGHLY based on the region where hunter-gatherers lived. For example, the Hadza get 15% of their year-round calorie intake from honey plus fruit sugar. [72] Other cultures with access to bodies of water consumed a diet higher in seafood as it was more available. [73] Yes, it is highly likely that many ancestral humans ate a sizable quantity of meat as a staple of their diet; some humans likely ate very little meat due to lack of availability based on location. This makes sense from an evolutionary perspective when you consider that human metabolism is exceptionally flexible and can accommodate various diets and survive.
It’s important to point out that much of this discussion centers around the idea that eating what our ancestors ate is likely optimal for health. We should point out that it is a pretty big assumption with disagreement amongst scientists about whether it has merit. [74] The idea that eating like our ancestors is optimal for health requires the assumption that our food choices & evolution were somewhat “ideal” rather than cobbled together by natural selection. Furthermore, the idea that diseases like atherosclerosis are confined only to modern man and did not exist amongst our ancestors appears to be untrue. [75] It is likely our ancestors ate what was available to them simply to survive. There were likely no debates about what was optimal to consume for health 10,000 years ago. Instead, the priority was finding energy-dense food sources to sustain them. We aren’t saying that a diet that attempts to mimic the ancestral human diet is terrible for you.
On the contrary, getting rid of most processed foods means most of the diet would come from foods with lower energy density and higher satiety indices. This certainly can be healthy, but there’s no evidence that it’s superior to a diet that controls calories but still includes foods that were not available to ancestral humans like whole grains and dairy. [76][77][78][79][80][81] When considering any dietary component, it’s fair to view it in the context of what our ancestors ate. Still, we should default to the research’s consensus regarding its safety and/or health benefits rather than speculation regarding what nature “intended” us to eat.
00:57:00 Claim: There is no real specific claim here, only speculation about the Carnivore Diet possibly helping prevent various autoimmune diseases that Paul implies may be caused by plant “toxins.”
Reality: There is very little literature on this particular topic as autoimmune diseases are not well understood. To invoke Hitchens’ Razor, “That which can be asserted without evidence, can be dismissed without evidence.” There are quite a few anecdotal reports of people (including Joe and Paul) who claim the Carnivore Diet helped various conditions they suffered from. This is what’s known as anecdotal evidence. I do not want to completely dismiss anecdotal evidence as some scientific discoveries have been based on anecdotes. Here is the problem with anecdotal evidence: some vegans make the same claims regarding autoimmune diseases. [82][83][84][85][86] What makes their anecdote less valid than Paul, Joe, or any other carnivore’s anecdote? Without empirical evidence, all that’s left is speculation. Paul claims that plant toxins may cause these autoimmune issues. Still, when we examine the literature on plant intake and autoimmune disorders, there appears to be no connection between the two as we could find no research indicating that plant intake increases the incidence of autoimmune diseases (we are open to rebuttal if Paul does indeed have citations). However, there is evidence that the gut microbiome may modulate autoimmune responses and that dietary fiber may improve autoimmune disorders.[87][88][89][90] Furthermore, vegetable intake was negatively associated with rheumatoid arthritis, an autoimmune condition. [91] Other dietary interventions that may positively affect various autoimmune disorders include reducing protein intake and replacing saturated fats (SFAs) with polyunsaturated fats (PUFAs), both of which oppose Paul’s recommendations. [92][93][94][95][96][97][98][99][100]
Moreover, the current western lifestyle is characterized by high fat intake, high calories, high intakes of processed foods, and minimal exercise. Many different diets might improve autoimmune diseases merely through improvements in overall health via departing from the current western lifestyle. [101] Indeed, there is evidence that caloric restriction, in general, improves autoimmune conditions. [102][103][104] Joe mentioned that he lost 12 lbs while on the Carnivore Diet and his vitiligo. Was this because Carnivore has some inherent property that makes it superior for treating autoimmune diseases, or was it the drastic reduction in calories that allowed him to lose 12 lbs in a month (an over 1000 calorie per day deficit)? This is why it’s crucial to rely on empirical evidence when making broad recommendations for populations. We cannot conclusively say that plants may not contain compounds that trigger autoimmune responses for some individuals, much like lactose-intolerant folks may have an immune response to dairy. At the same time, other people can consume it with no issues. There is, however, no evidence we are aware of to indicate plant consumption increases autoimmune disease incidence. The research regarding fiber demonstrates it may have a protective effect. Even if Paul or other individuals have found physiological benefits to their autoimmune disorders by eliminating plants from their diet, it is irresponsible to advise others to do so based on all of the other health benefits for the majority of people gleaned from plant/fiber consumption.
Furthermore, anecdotes are subject to the placebo effect or the power of suggestion. We already have consistent data showing that not only can placebo change the way we feel, but it can change our physiology. [105][106][107] Thus, many people claim to see benefits from various diets that are not supported by empirical evidence but may nevertheless have experienced those benefits due to the placebo effect if they felt very positively about the diet they self-selected. Sadly, skeptics like us will likely never experience the amazing benefits of placebo due to our understanding of its existence. All this to say, your experience is valuable to YOU but means very little on a population-wide recommendation basis.
01:03:30 Claim: “Both the men and the women in the Hadza tribe rate honey as their favorite food. And the men say meat is their second. The women say that meat, berries, and baobab are all…”
Reality: When Paul trails off talking about the food preferences of Hadza women, there is a reason for that: Hadza women prefer honey first, then berries, then baobab, then meat, which beats out only tubers. In another paper (“Sex Differences in Food Preferences…”), the same authors are explicit: “Hadza females ranked meat 4th out of five food types”.
What’s more, according to one world expert on the Hadza, while meat accounts for a whopping 40% of the calories in the diet among adult men, among women, this figure is only 1.2%, making Hadza women near-vegetarian. [108]

01:04:07 Claim: “At the end of the paper, they say that there is this observed behavior, that if there is a lot of meat in the camp, the women will stop digging tubers for 2-3 days.”
Reality: This paragraph says a lot more than that, but you wouldn’t know it if you only based your understanding of the Hadza diet on Paul’s claims on JRE. Here is that paragraph in full:
“Another reason the Hadza are able to avoid serious wasting is their ability to fall back on tubers. Women normally dig tubers every day though they may ignore tubers for an extended period when berries come into season since berries are superabundant. In addition to being more highly preferred (ranked 2nd by women), berries are easy to acquire. Children as young as 2 or 3 years old can simply feed themselves all day on berries and need little provisioning (Hawkes et al., 1995). Hadza women also occasionally skip digging for tubers for 2 or 3 days running when there is a lot of meat in camp. During the Plio-Pleistocene hunting was likely much less efficient so tubers would have been even more important to fall back on.”
In other words, a) Hadza women ignore tubers for an extended period when berries are available but occasionally skip digging for them when there is a lot of meat, a profound nuance that Paul neglected to mention and b) they prefer berries over meat; c) tubers were probably even more critical in the evolutionary past than they are today. This selective citation throws into relief Paul’s characteristic strategy of cherry-picking the research to “support” his views while ignoring research showing he is flat out wrong. Paul does this even to data within the same paper, indeed even within the same paragraph. The Hadza, who Paul repeatedly praises, consume something that is a far, far cry from the Carnivore Diet, as we shall soon see.
01:07:00 Claim: The differences in biochemistry—particularly with respect to rate-limiting enzyme phosphofructokinase—causes a person to be unable to consume too much glucose while being able to consume fructose endlessly.
Reality: This is an incredibly bizarre point because it tries to explain appetite based on glycolytic biochemistry. Satiety regulatory systems and glycolytic biochemistry are two entirely separate systems that are not known to interact. Yet, Paul somehow tries to derive an explanation for satiety from enzyme biochemistry. Fortunately, this exact question that Paul speculates upon has been studied several times in humans, and the results are the opposite of what Paul claims. Indeed, studies show that when subjects are fed fructose before a meal, they experience significantly greater satiety and eat fewer subsequent calories than when they are fed glucose. [109][110] The same goes for when they are fed sucrose before a meal, compared to glucose. [111]
These findings are the precise opposite of what Paul says. This should not be surprising: one cannot derive complex biological outputs by speculating about biochemical enzymatic regulation. This is a fundamental error betraying Paul’s lack of scientific literacy and familiarity with impartially evaluating scientific evidence.
01:08:01 Claim: High-fructose corn syrup short-circuits satiety mechanisms, while fruit does not, because of the stop-gap imposed by fruit.
Reality: This is a strange claim because fruit is also high in fructose, just as high-fructose corn syrup is. Fruit should, therefore, according to Paul’s biochemical explanation, be just as (un)satiating as high-fructose corn syrup, yet he claims that fruit isn’t. Which is it?
01:10:42 Claim: Paul claims that he is asking that people eat a “reimagined version of the Paleo diet” and that we are “still programmed to eat like our ancestors and will thrive doing so.”
Reality: Since Paul is so enamored with the Hadza, we can look and see just how congruent his claims are about the Carnivore Diet versus that consumed by that hunter-gatherer group. First, in one study, it is crucial to understand that meat constituted only about 20% of calories among all Hadza tribe members of all ages, a far cry from the diet consumed by Paul. What’s more, only 1.2% of calories among women 18 years or older were from meat, which is nearly a vegetarian diet (men consume the lion’s share of meat, for 40% of calories). [112] The rabbit hole goes deeper. A recent 2018 paper showed a by-calorie macronutrient breakdown in the Hadza diet of 24% protein, 65% carbohydrate, and 11% fat, [113] not dissimilar in fat content from the diets recommended by advocates for low-fat diets for cardiovascular disease [114] and the complete opposite of the ketogenic diet repeatedly praised by Paul throughout the interview (see, e.g., ). These estimates are consistent across historical time, noted by fieldworkers working as early as 1958-67: “Probably as much as 80 per cent of their food by weight is vegetable, while meat and honey together account for the remaining 20 per cent.” [115]
Similar estimates have been consistently provided ever since, using increasingly rigorous methodologies (x). What’s more, while Paul always decries the role of “seed oils,” unsaturated fat, and especially linoleic acid in the American diet (see, e.g., x, y, z), what he neglects to mention is the significant source of fat in the Hadza diet is the baobab seed. The baobab seed, which is ground into a kind of flour, provides, you guessed it, seed oils, which are rich in unsaturated fats and linoleic acid. Indeed, the baobab seed provides 62% of its fat from unsaturated fatty acids and 29% from saturated fatty acids. 25% of the total fat from the baobab is from linoleic acid. To make matters worse for Paul, the low-fat content of the Hadza diet, despite the 20% by-calorie meat intake, is due to the leanness of African wild game. [116][117]

Interestingly, even though wild game has low-fat content, the fats they have tend to be rich in PUFAs (>20%). [118] So while the Hadza diet is extremely low in fat compared to the standard American diet or ketogenic diets, the fatty acid composition of the fats therein is “seed oil.” All of which are unsaturated and linoleic acid-rich while being relatively low in saturated fat. It’s the exact opposite of Paul’s diet but consistent with current American dietary guidelines, which recommend replacing saturated fat with unsaturated fat. [119]
What about hunter-gatherers in general? While Paul’s favorite hunter-gatherer group may consume the absolute opposite of the diet that he consumes, perhaps other hunter-gatherer groups may consume something more like the so-called Carnivore Diet? The most well-known analysis of hunter-gatherer diet composition is Loren Cordain and colleagues’, conducted using Murdock’s Ethnographic Atlas. In their analysis, they appeared to have demonstrated that most of the 229 hunter-gatherer societies studied for the Atlas (73%) consumed more than 50% of their energy in the form of animal foods. In contrast, only 13.5% of such groups consumed more than half of their energy from plants. While this would not support a Carnivore Diet, it would be consistent with a diet high in animal foods.
There are several problems with Cordain et al.’s interpretations. First, most of the Atlas data was not collected by people with training in dietary collection techniques. [120] Second, the Atlas is compiled from mostly 20th-century sources, and most remaining hunter-gatherers in the 20th century had been displaced to marginal environments. Therefore, their diets are not representative of our hunter-gatherer ancestors. [121] Third, most of the so-called hunter-gatherers were “casual” agriculturalists or mounted hunters with guns. When these are excluded, only about 10% of hunter-gatherers remain. [122] Fourth, the Atlas “in almost all cases represents subjective approximations by Murdock of the ethnographer’s or anthropologist’s original observations.” [123] Fifth, the data were collected by men, who often did not associate with women, who typically collect and process plant resources. [124]
When Lee studied the Atlas in 1968, he included only true 24 hunter-gatherer societies and came to strikingly different conclusions from Cordain et al., which Cordain et al. did not mention in their discussion. But perhaps more importantly, while the early development of the so-called diseases of civilization has not been documented in any hunter-gatherer group, this was the case regardless of whether the diet was based predominantly on plants or animals, suggesting that the animal or plant predominance of the diet is irrelevant to health. This indicates that Paul’s plant phobia is simply an irrelevant factor, at best, when it comes to achieving optimal health. Katherine Milton concludes her commentary on the Cordain analysis by noting: “a high dietary protein intake is often accompanied by high saturated fat and cholesterol intakes.” Given that most Westerners do not have access to wild game, this recommendation seems prudent.” What is clear is that our ancestors didn’t often consume fatty ruminant meat, the kind on which Paul hangs his hat.
01:32:40 Claim: Paul says people take his desiccated organ supplements and tell him they feel better
Reality: It’s possible they feel better if they were experiencing some sort of nutritional deficiency, but they could have likely corrected this with a regular vitamin and mineral supplement. Supplementing above and beyond dietary recommendations with vitamins and minerals typically doesn’t show much benefit. [125] Also, see our previous discussion on the placebo effect.
01:40:10 Claim: “We were eating way more saturated fat in 1900 than we are today, so to say that saturated fat is driving this doesn’t make a whole lot of sense.”
Reality: This claim is about an increase in cardiovascular disease primarily over the last 100 years. While Paul is correct that the RELATIVE contribution of SFAs has decreased since 1900 (43% of fat intake to 30% of fat intake), the TOTAL intake of fats has increased by approximately 50%, which means the intake of SFA on an absolute basis has increased significantly. [126] Further, it’s impossible to separate the increase in CVD from the rise in the obesity epidemic, which drastically increases CVD risk independent of any other factors. [127][128][129] Therefore, both the rise in SFA and the increased caloric consumption contributing to increased obesity rates may have simultaneously increased CVD rates.
It’s also worth pointing out that Paul is once again picking and choosing where he uses various pieces of logic. Essentially what he is doing right now is discussing epidemiology. What one group ate vs. what another group ate vs. their risk of a certain disease. But Paul has repeatedly claimed that epidemiology is “garbage” or claimed that it’s not reliable. [130][131] Does epidemiology have its limitations? ABSOLUTELY. But if you are going to claim it’s garbage, you can’t then invoke associations when they fit the narrative you are pushing if you wish to be logically consistent. As we have repeatedly observed, however, Paul uses and discards various pieces of logic as it suits his agenda.
01:41:00 Claim: This is a long ramble, but essentially Paul attempts to connect PUFAs to lipid peroxidation, to oxidative stress, then to CVD. There is then some discussion on LDL formation and why LDL is unfairly demonized.
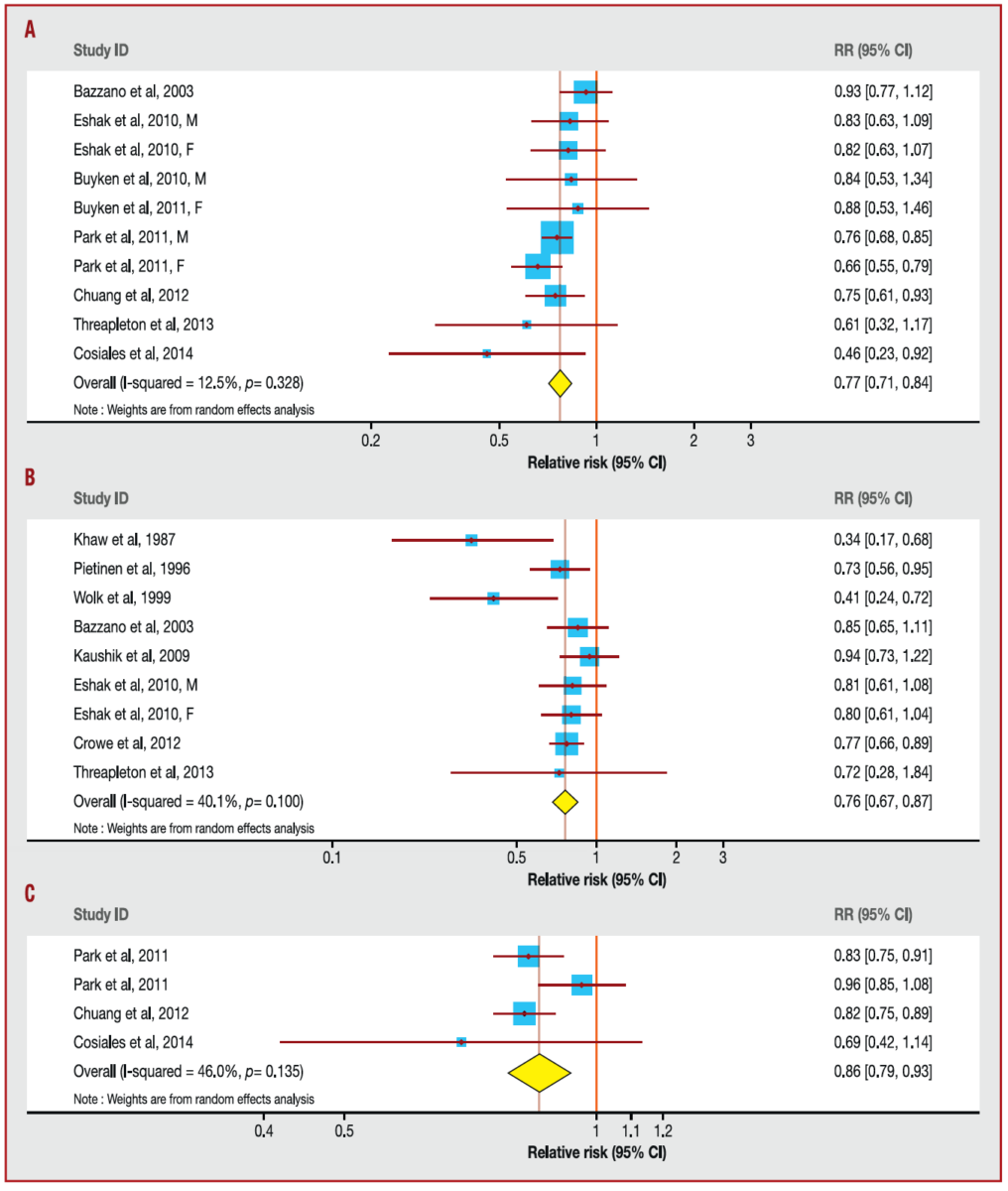
Reality: One big problem with this attempt to connect PUFAs to heart disease, the actual outcome evidence does not support it; in fact, it strongly supports the opposite. Replacement of SFAs with PUFAs has a consistent protective effect on CVD. [132][133] This is likely due to a few different mechanisms, the first being that SFAs reliably increase blood LDL cholesterol levels and by default Apolipoprotein B (ApoB) which is thought to be a major factor contributing to atherosclerosis and CVD (more discussion on this later). [134][135] Replacement of SFAs with PUFAs (particularly omega-3 PUFAs) has been shown to have a protective effect on CVD, likely by lowering LDL, ApoB, reducing inflammation, and various other proposed mechanisms. [136] This even holds true in a meta-analysis of CVD risk and linoleic acid intake, which is the particular PUFA that Paul tries to blame for CVD and obesity. [137][138][139][140] Much of Paul’s position is based on the lack of randomized control trials demonstrating an effect of replacing SFA with PUFA on CVD outcomes (although omega 3 PUFAs do appear to reduce risk in RCTs). [141][142][143] Part of the problem with attempting RCTs when studying something like CVD is the lack of capturing lifetime exposure risk. Atherosclerosis/CVD is not something that develops quickly; it develops throughout a lifetime. [144] A randomized controlled trial is difficult to run for long periods. It requires much time, money, and patience. Not only that, the subjects and researchers must also stay committed. In a meta-analysis showing no benefit in RCTs where PUFAs were increased, and SFAs decreased, the longest trial was 8 years, and most were 2-5 years. [145] Additionally, most of these trials were performed on people who already suffered from heart disease. So what this data likely means is that amongst people who already have damage to the vascular system, replacing SFA with PUFA doesn’t seem to do much in the short term. Most of the people in these studies are 60 years or older, and they are only monitored for around ~5 years post-intervention. For perspective, 5 years is less than 10% of their lifetime, whereas their LIFETIME exposure determines their risk. While randomized controlled trials are the gold standard in research, we cannot neglect their limitations, especially when it comes to subject number and time duration. Compare this with the cohort studies on the effects of replacing SFA with PUFA that demonstrate quite a powerful protective effect of replacing SFA with PUFA that appears to be dose dependent. [146] Further, even when specifically looking at omega 6 PUFAs, which Paul claims are unhealthy, there is a protective effect when replacing SFA with them. [147][148] In this cohort study, those with higher blood levels of omega 6 PUFAs had a 50% lower risk of a CVD incident during a 35 year follow up.
A good analogy for understanding lifetime exposure risk would be thinking about it as we think of investing. Let’s compare what would happen if we invested $2000 every year for 40 years in an investment that made either an 8% return or a 6% return. After a year, if we examine our investment, we will be unimpressed with the differences. There will only be a $60 difference ($2160 total vs. $2120). Based on that single year, we might say that there is no practical difference between those investments due to such a small difference. Even after 5 years of investing $2000 every year, we’d only see a difference of $721.22 even though we’d have invested $10,000. But as time went on, we’d start to see a drastic separation between the two investments: After 15 years, the difference would be $9,303.51, and after 30 years, the difference would be an incredible $77,088.39. At 40 years of investing, the difference would be $231,466.71. Think about your diet choice and risk of developing heart disease like an investment. In the short term, it won’t likely matter much unless you do something extreme, but in the long term, it makes a very significant difference.

For argument’s sake, let’s say that PUFA does not have a protective effect on CVD. Remember, Paul is attempting to connect PUFA, particularly LA, to CVD. But when we look at the actual outcome data, no hard data is supporting his claim. Even the meta-analysis of RCTs that didn’t show a beneficial effect of replacing SFA with PUFA certainly did not show a negative effect. So while there is a lot of evidence to suggest replacing SFA with PUFA may reduce CVD events and a little bit suggesting that it might not be protective, NO hard data is demonstrating that PUFA increases CVD events. What Paul is doing is attempting to isolate a specific nutrient, then find a mechanism to connect it to disease. This can be done with virtually any nutrient. His logic is PUFA can be oxidized —> oxidation can damage the arteries —> damaged arteries can lead to CVD. Once again, his logic is not consistent. Saturated fat increases LDL cholesterol, which Paul claims is not bad for us, but LDL, which has been demonstrated to damage the arterial wall. [149][150][151] Paul also neglects to mention LDL itself is subject to oxidation, which can increase damage to the arterial wall. [152] Not only is there a mechanism for disease progression, but there are also HARD clinical outcomes of people who have higher LDL showing a greater incidence of CVD. [153][154]
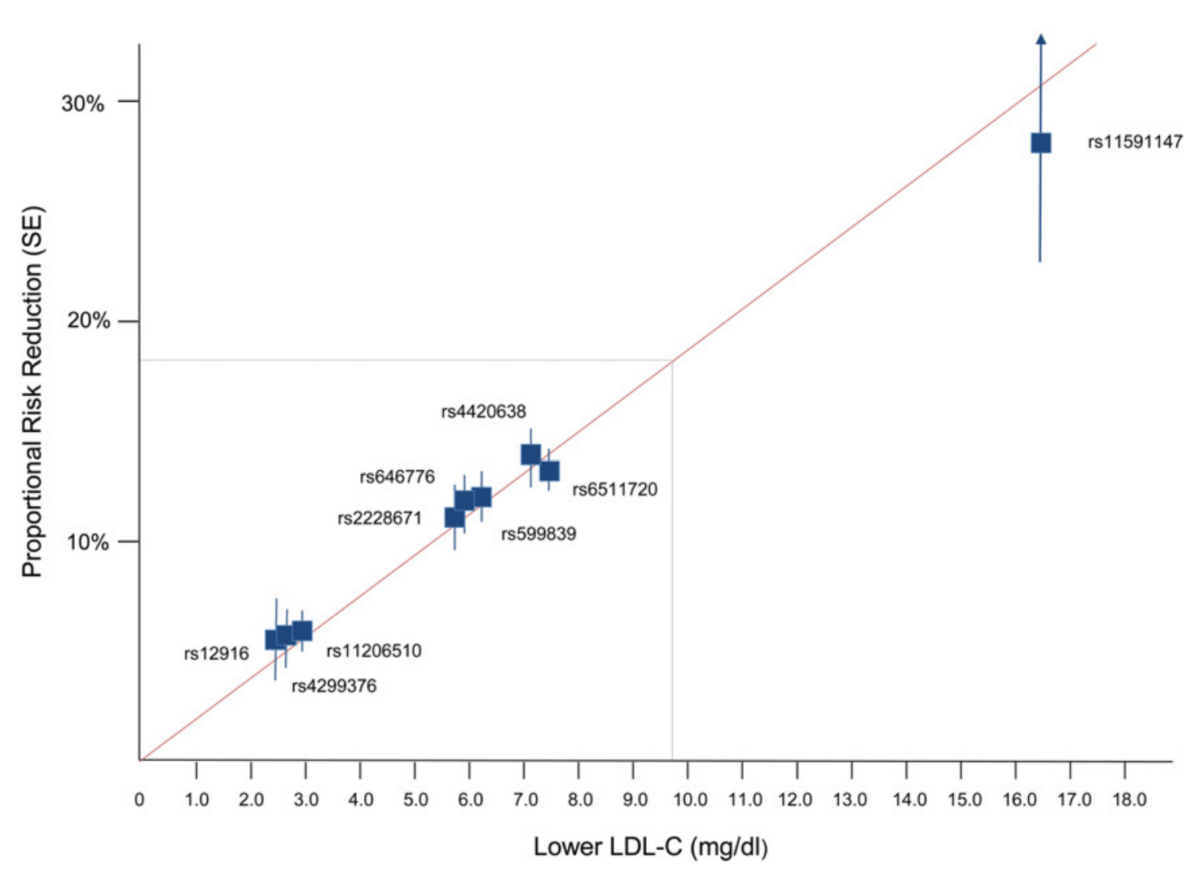
Not only do we have this hard outcome data, but perhaps the most robust evidence for LDL causality on CVD is the Mendelian randomization (MR) studies. MR is interesting because it essentially allows a randomized controlled trial over a long period. In many ways, MR is more tightly controlled than traditional RCTs. Briefly, MR studies take advantage of our genetic diversity and polymorphisms. Various subsets of our population will have genetic polymorphisms that cause them to naturally have higher or lower LDL levels while other blood lipids remain unaffected. [155]
By stratifying them into these various groups and looking at CVD incidence, we can determine whether or not LDL is causative rather than just associated with CVD. Keep in mind that this is, for all intents and purposes, a lifetime RCT, where people are exposed to varying levels of LDL based on their genetic differences. If LDL were only associated with CVD, rather than causative, we would expect to see random results if it’s genuinely all just “healthy user bias” as Paul claimed due to the natural randomization.
What we find is that in virtually ALL MR studies is a linear relationship between blood LDL levels and CVD incidence, indicating a causal relationship. [156][157][158][159][160] Not only that, but the reduction in CVD incidence from low LDL levels was GREATER than predicted. [161] Finally, this effect of LDL on CVD holds even with varying HDL levels, TAGs, and inflammation. For example, at high or low levels of inflammation, people with lower LDL cholesterol have a lower risk of CVD compared to people with higher levels of LDL. [162] That is, amongst people with low inflammation and either high or low LDL, the people with low LDL have a lower CVD risk. Amongst people with high inflammation, people who have low LDL have a lower risk of CVD than those with more elevated LDL. The same holds for HDL as well as MR studies on HDL have not shown a protective effect on CVD. [163][164] This is consistent with data demonstrating that drugs which raise HDL do not protect against CVD. [165]
I’m not saying that you can’t have modestly high LDL and be relatively low risk for CVD. Indeed, if you have modestly high LDL, high HDL, low TAG, lean, exercise, don’t smoke, have low inflammation markers, good blood glucose control, and live an otherwise healthy lifestyle, your absolute risk of CVD may be pretty low. But is it as low as it would be if you had all those things PLUS low LDL? Not based on the data, as the MR studies consistently show that people with the lowest LDL levels consistently have a lower risk of CVD across varying levels of inflammation, HDL, and TAGs.
All of this to bring it back to the topic of Paul’s claims that saturated fat is good for you while PUFAs are bad. [166] There is no hard evidence to back this up, and Paul’s logic isn’t even consistent. He attempts to draw a mechanistic link between PUFA oxidation and CVD while ignoring the fact that saturated fat has a much STRONGER mechanistic link to CVD, which is backed up by actual outcome data in humans. He’s asking you to focus on a tree instead of the forest. Meanwhile, we not only have mechanistic data showing saturated fat can damage the arterial wall, but we also have outcome data and MR data across multiple lines of evidence showing saturated fat and LDL are most likely causal for CVD. There is no evidence that I am aware of demonstrating that PUFAs are casual for CVD, and if anything, they likely have a protective effect.
01:44:05 Claim: “There are so many studies that point to the value of LDL, and if we just think about it from an evolutionary perspective, why would nature have designed a particle within our body that kills us?” This statement is made after Paul discusses how children born with a genetic error where they do not make cholesterol have all kinds of health problems.
Reality: This once again is Paul picking and choosing how he uses logic. The argument he is attempting to make here is that since these individuals can’t make LDL and have all these health problems, that must mean LDL is good for us. What if we couldn’t make glucose? That would be horrible for us. In fact, it would kill most of us from severe hypoglycemia if we went any length of time without eating carbohydrates. By that logic, shouldn’t we be concerned about my daily intake of carbohydrates? Do you see how this logic falls apart when we flip it?
Further, the vast majority of nutrients have safe ranges of intake and have adverse effects when overconsumed; this is the basis upon which the concept of the DRI (daily reference intake) ranges was developed. Sure, if you altogether remove any nutrient, it’s likely not going to be good, but keep in mind that cholesterol, much like glucose, can be synthesized just fine from non-cholesterol substrates in the liver. Just because people with an inborn error where they don’t make cholesterol have health problems means absolutely NOTHING for those who can.
As for the “Why would nature have designed a particle that kills us?” comment, we aren’t sure if Paul is serious about this. Is he aware of how many particles made by our body will kill us if they are too high? Glucose, for example. Extremely high blood glucose levels are toxic and will kill us, yet our bodies have developed elaborate systems for metabolizing glucose. [167] Our bodies also make ammonia, which could kill us if not handled correctly. [168] Methanol is synthesized by our gut microbiome but is also lethal in high doses. [169] That said, let’s grant his “logic” an audience. Try to think about the purpose of life from an evolutionary perspective. The purpose of life is to survive long enough so that we can pass on our genetic material. Evolution is not concerned with us surviving to the ripe old age of 80. We evolved to survive famine. We needed to develop elaborate metabolic systems to capture various forms of energy from sources like proteins, carbohydrates, and fats.
Our bodies did not evolve to synthesize LDL cholesterol to kill us. Quite the contrary, our body’s handling of lipids was developed to keep us alive and resist famine. However, now that famine is no longer an issue, we are dealing with the evolutionary fallout of that system. High LDL levels don’t kill you in a month, a year, or even a decade. They might be the difference between living to 67 and 75 on average. [170] From an evolutionary perspective, biology could care less about which age we die since the transmission of genetic material would have already occurred long ago. So even if Paul’s argument wasn’t ridiculous since our body synthesizes many compounds that will kill us (and much faster than LDL, I might add), the argument falls apart when you consider evolutionary biology’s purpose.
Finally, this idea that there is a minimum LDL level we need to be healthy is reductive. You could make a much stronger argument for a minimum level of glucose for survival, that doesn’t mean it’s a great idea to have chronically high blood glucose. Yes, with zero LDL cholesterol, we’d have big-time issues, but the amount needed to survive is extremely minimal. The original work on the LDL receptor found that it became saturated at 2.5mg/dl. [171] This means that the physiological maximum for total circulating cholesterol is around that level, and any additional cholesterol is SURPLUS to cellular requirements. So Paul’s attempt to convince us that LDL is good for us and that we don’t want to lower it too much because people without LDL would have health problems is complete NONSENSE. 100mg/dl would be around 40 times more LDL than you require. Imagine if someone was implying that glucose was good because we’d have health problems if we didn’t have any in our blood? It’s LITERALLY the SAME argument.
Further, in recent statin trials where people with already low LDL (~100mg/dl) are placed on statins that lower it even further (STILL see an over 50% reduction in CVD incidence. [172] During development as an infant, when growth is at its most rapid, our LDL levels are around 70mg/dl, more than enough to support growth. [173] Current recommendations for LDL levels to reduce heart disease risk are [174] There is no hard evidence that lowering LDL to these amounts will negatively impact health in any way. His logic that we don’t want to lower LDL because people with genetic mutations in the LDL receptor get sick is RIDICULOUS.
01:45:10 Claim: “LDL helps protect us against infection because it’s part of the immune system.” Paul made this claim after discussing that knocking out the LDL receptor in rodents led to better resistance against infection, and epidemiology studies show higher infection rates in people with low LDL.
Reality: He is correct insofar as his statements about rodents with knockout LDL receptors & infection as well as the epidemiology studies. What he is leaving out is that trying to equate a rodent knockout model with real human metabolism is ridiculous, and there are thousands of examples where this doesn’t carry over. There is no comparison between a rodent with no LDL receptor and someone who eats a diet that modifies their LDL. While these mice have lower rates of infection, he also left out the part where they have higher rates of non-alcoholic fatty liver, CVD, obesity, impaired cognitive function, type 2 diabetes, and a whole host of other health problems compared to normal mice…Why didn’t he mention those? [175][176][177][178] This is another example of Paul cherry-picking. He talks about LDL receptor knockout mice when it supports his argument but doesn’t talk about all the other animals’ problems.
Furthermore, while high HDL and LDL are inversely associated with infection risk, only HDL appears to have a causal effect on reducing infection risk. In contrast, LDL has no effect, based on Mendelian randomized (MR) trials. [179]
01:47:08 Claim: “Epidemiology can generate correlation, but we cannot draw causative inference from that data.”
Reality: This is the only thing Paul has said that we agree with thus far. That being said, please note all the times that Paul invokes epidemiology (typically cherry-picked) to support his points, including 2 minutes prior.
01:48:26 Claim: The lipid hypothesis is incomplete because it doesn’t account for HDL (I’m paraphrasing, but this is accurate based on what he said). He shows a chart from the Framingham study where CVD risk was drastically reduced with high HDL even in people with high LDL.
Reality: HDL is indeed associated with decreased CVD and improved metabolic health. [180][181] In fact, it was long thought that LDL wasn’t so much the problem as the ratio of LDL to HDL. I was a big believer in this up until a few years ago. However, it’s unlikely that HDL has a role in CVD other than being an indicator of better overall health. As we stated previously, drugs that raise HDL have had remarkably disappointing results for reducing CVD risk. [182] This is also supported by MR studies which have failed to demonstrate a protective effect of natural elevations in HDL on CVD. [183] Furthermore, even if (and that’s a big “if” based on current data) HDL was protective on CVD, that does NOT exonerate LDL as an independent risk factor.
As we discussed previously, even in people with high HDL levels, if they also have low LDL, they are MORE protected against CVD than people who have high HDL and high LDL. [184] It’s important to note that the data demonstrating that high LDL is associated with higher CVD rates at both low HDL and high HDL came from the SAME DATASET (Framingham) that Paul displayed onscreen during the podcast. This means he either did not examine this portion of the data set or purposefully omitted it. That doesn’t mean we should not try to raise HDL; as we previously said, it may have a protective effect on infection.
01:50:08 Claim: Joe asks Paul if the problem is not high LDL but low HDL, and Paul says the issue is metabolic dysfunction and insulin resistance. We use HDL as a proxy marker of metabolic health.
Reality: Insulin resistance increases CVD risk and all-cause mortality, but this is a strawman argument by Paul. [185][186] Once again, just because insulin resistance increases CVD risk does NOT absolve LDL of being an independent risk factor for causing CVD. Perhaps even more interestingly, LDL may be a causative contributor to insulin resistance itself. [187] Interestingly, modifying HDL does not appear to reduce the risk of type 2 diabetes. [188] Paul’s argument falls apart when we examine CVD risk amongst people with type 2 diabetes. Researchers observe that LDL is still an independent risk factor for CVD in this population, even when other variables are accounted for. [189]
If LDL was not a causative factor for CVD and the issue was simply insulin resistance, then we’d expect to see no difference in CVD rates amongst people with type 2 diabetes based on their LDL levels, but we do. As it turns out, LDL may contribute to the development of insulin resistance. Furthermore, in people with type 2 diabetes, increasing LDL appears to have an even more potent effect on increasing CVD risk than in non-type 2 diabetes populations. [190] This could explain the tie in between elevated LDL levels, type 2 diabetes, and CVD.
01:51:08 Claim: LDL Cholesterol alone is too simplistic a metric (to explain heart disease). “I don’t believe that high LDL in someone whose metabolically healthy is the same as high LDL in someone who is metabolically unhealthy.”
Reality: Paul is right. Heart disease is not only caused by LDL. High LDL in someone healthy does not have the same risk as high LDL in someone who is metabolically unhealthy. That still does not absolve LDL as an independent contributor to the development of CVD as we have so painstakingly spelled out already. People with high LDL but low inflammation and high HDL STILL have greater CVD risk than those with low inflammation, high HDL, AND low LDL. [191][192] Paul fails to understand what an “independent risk factor” means. An independent risk factor does NOT mean that it is the ONLY risk factor, and it does NOT mean that other risk factors don’t matter. There are other independent risk factors such as obesity, insulin resistance, and smoking. Just because LDL can’t explain the TOTALITY of CVD risk does not mean it is not an independent risk factor that does CONTRIBUTE to someone’s overall risk.
I’m sure Paul would use the example of someone like himself who exercises, doesn’t smoke, doesn’t overeat calories, and claims that his risk of CVD is low despite his high LDL, and he’s PROBABLY RIGHT. But his risk is still NOT as low as someone who has all the same characteristics PLUS low LDL. These are risk factors that summate. He is creating the “unicorn fallacy” whereby if something isn’t perfect, it is worthless. LDL cannot perfectly explain the TOTALITY of CVD risk throughout a lifetime, but it DOES explain at least part of that risk based on the data. This would like me saying that speeding is not a risk factor for a fatal car accident because I don’t text while driving, don’t drink and drive, and I wear my seatbelt. Is my overall risk low because I’m doing most things correctly? Probably. Is it as low as it could be if I didn’t drive so fast? No. [193]
01:52:00 Claim: Fasting bears have a rise in LDL, but they don’t develop atherosclerosis.
Reality: I suppose that’s great news. For bears, I mean. As for humans, yes, LDL slightly rises when you begin to fast. That is a fuel mobilization response, nothing more. LDL levels quickly start to decline during a prolonged fast and continue to decline as more weight is lost. [195][196] Paul is attempting to use this point as a workaround to show why LDL is good for you. I.e., fasting is good (it isn’t always), and fasting raises LDL, so, therefore, LDL must be good, right? Based on everything we discussed previously, plus the fact that the elevation is only transient, quickly falling back down, the answer is no.
Shortly thereafter, Paul makes the GARGANTUAN LEAP by saying that “You’re telling me this thing (fasting) that happens naturally is killing us in a way? That’s causing atherosclerosis? That doesn’t make any sense.” No, Paul, what does not make sense is your inability to grasp a short term change in energy flux compared to LONG TERM EXPOSURE to chronically elevated LDL levels. As we already discussed, the LDL rise to fasting is a few days/weeks at MOST before it returns to normal and falls as weight is lost. Once again, Paul is making a strawman of the lipid hypothesis. NO ONE is saying fasting will cause atherosclerosis. Scientists say that based upon MULTIPLE LINES of evidence across epidemiology, animal models, mechanistic data, human intervention trials, MR studies, systematic reviews, and meta-analysis that CHRONIC elevations in LDL are very likely to contribute to causing CVD.
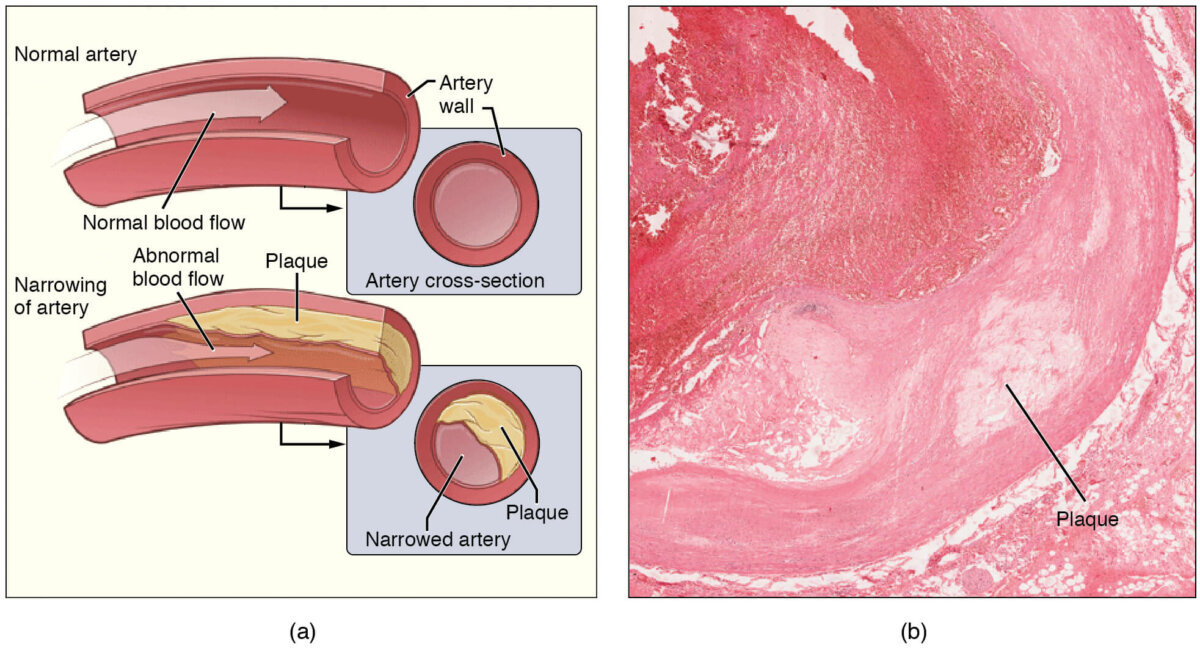
01:54:34 Claim: If LDL causes atherosclerosis, why do we only get it in arteries and not veins? It’s all part of our circulatory system, and it’s continuous.
Reality: You could make this argument for ANY risk factor of CVD, including smoking and oxidative stress. The reason that we do not develop atherosclerosis in our veins compared to our arteries is that the arteries are a much more high-pressure system, which increases the deposition of plaque. In contrast, veins are not high pressure enough to cause deposition. [197] In animals with artery grafts transplanted into the venous system, the arteries do not accumulate plaque, but when a vein is transplanted into the arterial system, it can accumulate plaque. [198] This is not unique to LDL cholesterol, as Paul is trying to make it seem.
01:57:16 Claim: “Within the framework of healthy lipid metabolism, there is no evidence that elevated LDL leads to atherosclerosis.”
Reality: This is PATENTLY FALSE based on the multiple lines of evidence we discussed previously. He also claims you can’t use familial hypercholesterolemia as evidence that LDL causes CVD because it “changes lipid metabolism.” He never discusses how it changes lipid metabolism or why that means you can’t use it as evidence. Even so, the MR studies where people have genetic polymorphisms that cause them to naturally have higher or lower LDL cholesterol demonstrate consistent increases in risk with more elevated LDL. In these studies, the genetic polymorphisms do NOT affect other aspects of lipid metabolism or change levels of other lipids such as HDL or TAGs. [199][200] So, his statement that there is no evidence is utterly false.
Paul also talks about how his LDL has been over 300mg/dl for 2 years, as if that anecdote is somehow validation that LDL doesn’t cause CVD. To be clear, LDL risk is due to LIFETIME exposure. So, 2 years of high LDL is unlikely to cause CVD in that timeframe, but over time, it has been shown to be a contributing factor to causing CVD.
Paul does say something I kind of agree with insofar as he says (paraphrasing) that if someone lost a lot of weight on a high meat diet and got much more metabolically healthy but still had high LDL, they would be much lower risk than before. He’s likely correct. But would they have reduced their risk as much as they would have had they lost that weight AND lowered their LDL? No, not based on the evidence. That being said, if the ONLY way that someone was able to adhere to a diet was an all-meat diet and that diet helped them lose a lot of weight, then maybe it’s better than the alternative. But I think most people could find a healthy middle ground where they can include meat as part of a healthy diet while limiting saturated fat, thus attaining weight loss, metabolic health, AND reduced LDL, and benefitting from those effects.
02:01:07 Claim: LDL can be good. It has all these roles; it’s protective in the immune system; it carries nutrients around the body.
Reality: Like glucose, a minimum level of LDL is required (far below what is achievable through diet, lifestyle, and even pharmaceutical interventions) to function. That does NOT mean surplus LDL has additional benefits. As we have repeatedly shown, it doesn’t, and it likely has deleterious effects on metabolic health.
02:01:55 Claim: “In the setting of metabolic dysfunction, the LDL, and this is just my hypothesis, I don’t think anyone knows this, perhaps the LDL gets retained (in the endothelium).”
Reality: All cardiologists and lipid researchers can go home; apparently, Paul has figured out the secret sauce of what causes CVD. I almost gave myself a lobotomy from rolling my eyes so hard. Paul is attempting to portray LDL as an inert passenger in the context of atherosclerosis (accumulation of plaque in the arteries). He says that the damage to the artery’s endothelium and the ensuing plaque build-up is caused by “metabolic dysfunction” (nebulous term). Only then does LDL begin to accumulate. But we KNOW from a lot of mechanistic data that LDL (especially oxidized LDL) can easily penetrate the arterial wall, damage it, recruit macrophages (inflammation), and initiate plaque accumulation and therefore is NOT passive, but rather causative. [201][202][203]
02:03:23 Claim: Paul finally acknowledges that LDL is causative (in a roundabout way) by acknowledging that oxidized LDL can damage the endothelium. He then speculates about how LDL is oxidized, saying that there is ”good evidence that linoleic acid does it,” then says oxidative stress may do it.
Reality: Yes, oxidized LDL can damage the endothelium. Thanks, Paul. He acts like this is not an inherent LDL property, and that oxidized LDL is a rare occurrence. The reality is that LDL is quite easily oxidized in healthy individuals in the ABSENCE of metabolic dysfunction. [204][205][206] That said, metabolic syndrome—I can only assume this is what he means by the nebulous term “dysfunction”—can exacerbate LDL oxidation. [207] However, it’s possible that LDL oxidation CONTRIBUTES to metabolic syndrome rather than the other way around as decreasing LDL oxidation IMPROVES insulin sensitivity. [208] As for his claim that Linoleic acid increases LDL oxidation? This claim likely comes from correlation data indicating that linoleic acid is associated with LDL oxidation. [209]
It’s important to remember that metabolism is complicated, and correlation cannot prove causation. Correlation can only be used to support intervention data as well as mechanistic data. What we are looking for is correlation data, mechanistic data, and OUTCOME data to all line up in similar directions, which is what we see with LDL as a causative factor for CVD. If we look at people who eat high amounts of linoleic acid, we simply don’t see an increase in CVD or atherosclerosis. We see the opposite. [210][211][212][213][214][215] I don’t want to dismiss the correlation between linoleic acid and LDL oxidation completely, as it does merit further investigation, but the fact that the actual OUTCOME data points in the opposite direction make Paul’s claim extremely weak. LDL appears to be oxidized just fine without any assistance in healthy people.
Paul then cites the Minnesota Coronary Experiment to justify why vegetable oils and PUFAs are harmful to you. The MCE took place from 1968-1973 in nursing homes where participants were fed a diet low in saturated fat and high in PUFA (9% SFA & 15% PUFA) or a diet low in PUFA & high in SFA (18% SFA & 5% PUFA). The average participant was on the diet for approximately 1 year (the mean was 384 days) and varied in age from less than 30 years old (this was the most popular age demographic, comprising ~20% of the total participants) to over 80 years old. What’s interesting about this study is that it was conducted in mental institutions and nursing homes where meals were provided to the participants, thus effectively being a rigorous randomized control. Paul claims that the low saturated fat, high PUFA diet did far worse, but this is simply not true. The finding from the study was there was no difference between the groups in coronary events. [216] That said, as we discussed previously, atherosclerosis does not appear overnight. Many participants were healthy young subjects and unlikely to have any cardiac event in the 1-year timeframe that the average person in the study participated. Over 52% of the subjects were UNDER the age of 50 and were otherwise healthy when they entered the study.
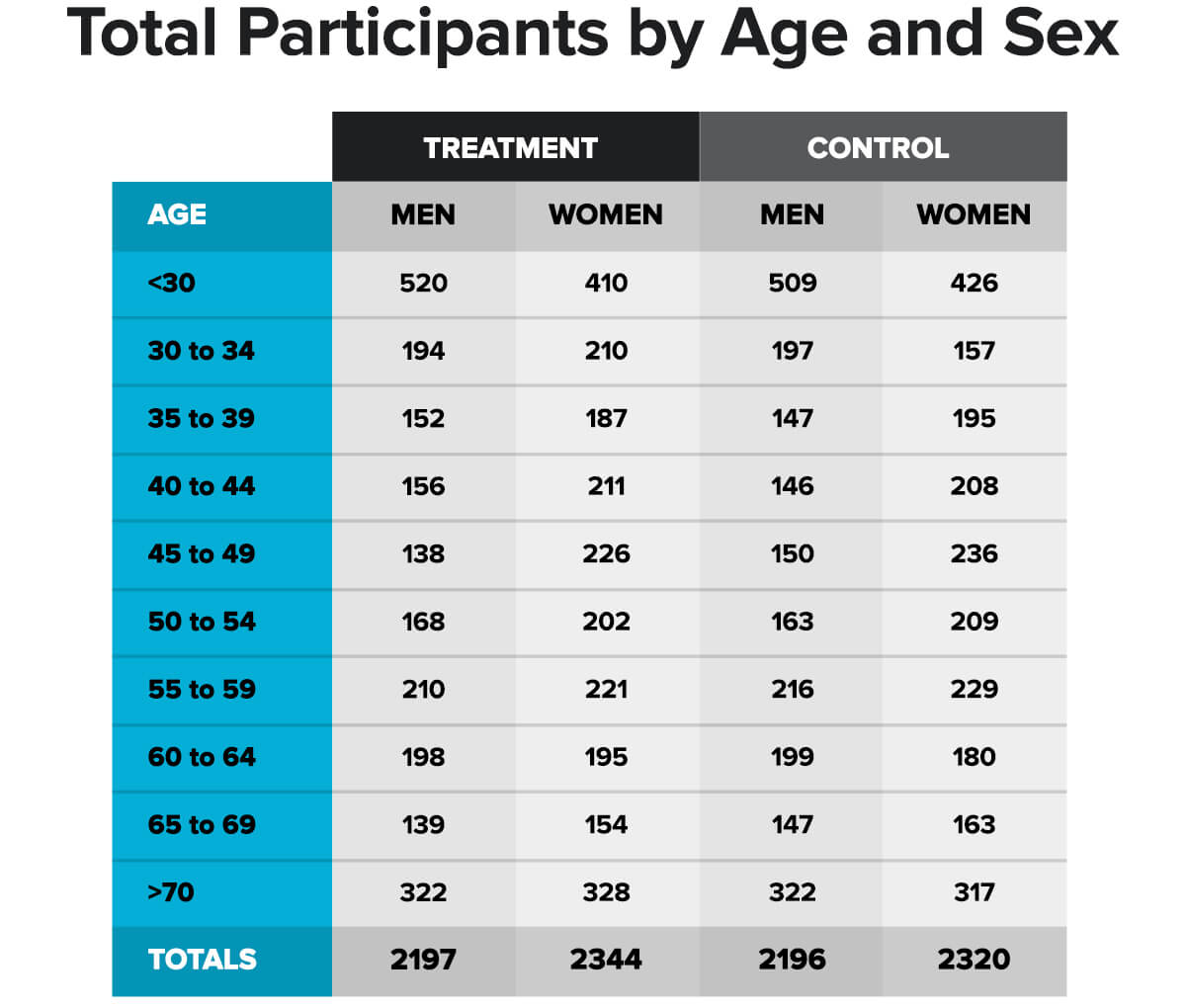
Table shows the ages and sex of the participants of the Minnesota Coronary Experiment. The control group was the normal SFA/PUFA group and the treatment group was the low SFA/high PUFA group
So, are you telling me that mostly young people ate these different diets for about a year, and there was no difference in CVD events? Color me shocked.
Remember that CVD events are a lifetime exposure risk, which is why we see ROBUST outcomes for LDL causing CVD in MR studies because MR is effectively a lifelong randomized control trial. [217][218][219] It is unsurprising that the researchers found no difference between the groups in this study. However, upon re-analysis of the data, of the people in the study who were age 35-55 and on the diets for more than 2 years, there was a trend for lower incidence of CVD events in the treatment group (low SFA, high PUFA). [220] Paul either is not aware of this analysis or purposefully omits it.
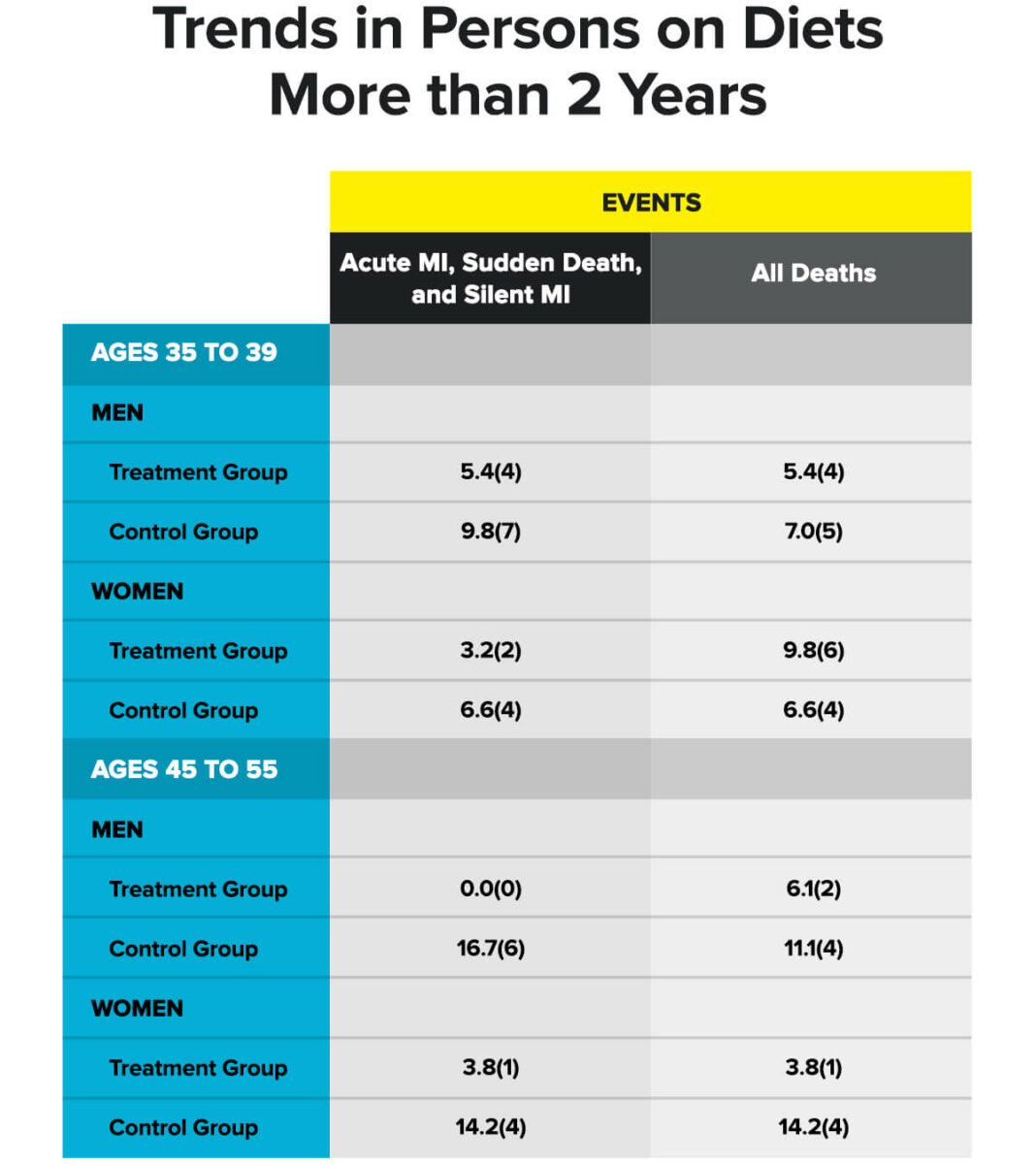
Table shows all myocardial infarction (MI) events and deaths in participants ages 35-55 years old. Values are expressed as number of events per thousand person-years. Raw event/death data is shown in parenthesis.
Keep in mind the age group is important. People who started the diet in this age group and stayed on it for a long time were young enough to likely start seeing benefits, but also old enough where we would begin to see some CVD events. In older people placed on statins, we don’t see a huge extension of lifespan due to lowering LDL, likely because they’ve had such a long lifetime of exposure that any treatment will likely only have modest effects.
If you follow younger people (age 30 or less) for 5-10 years, it’s unlikely even the most unhealthy of them will experience CVD. Therefore, population matters when you are testing CVD related outcomes. If we look at statin trials of 5+ years, we see a 30-50% decrease in risk of CVD events (interestingly, this holds true REGARDLESS of the mechanism of lowering LDL; the outcomes are similar if comparable levels of LDL are achieved), and that becomes even more powerful when we examine MR experiments that compare people with naturally high LDL vs. those with naturally low LDL. [221][222]
Data from a meta-analysis of MR studies demonstrate a 3-FOLD GREATER risk reduction in patients achieving lowered levels of LDL compared to those who reached similar levels of LDL but doing so by starting a statin later in life. [223] This demonstrates just how powerful the concept of LIFETIME EXPOSURE RISK is. Not only does it matter how low you get your LDL, but it also matters how long it’s at that level. To make it more visually appealing, check out this graph of risk reduction in 186,000 subjects from MR studies with genetic polymorphisms that cause them to have naturally lower levels of LDL. [224]
Log-Linear Effect of Each Unit Long-Term Exposure to Lower LDL-C on Risk of CHD
Figure demonstrates a linear reduction in lifetime risk of CVD event based on reduced LDL levels based on MR studies. I want you to imagine that a component of plants showed this same association with disease and think about if Paul would claim it is causative for said disease or not.
You see almost a perfectly linear association between the risk reduction and the amount of reduced lifetime LDL exposure. Now, look at the amount of LDL reduction needed to achieve this. Nearly a 30% reduction in risk by simply reducing LDL by around ~16.5mg/dl. In a similar analysis of 312,321 subjects in an MR study, the researchers observed a 54.5% risk reduction for every 38.7mg/dl of lowered LDL. That is incredible. Again, remember that MR studies can assess the effects of only changing LDL without affecting HDL, TAGs, inflammation, or insulin sensitivity. They can assess it throughout a lifetime… a LIFETIME randomized control trial! If this isn’t enough to convince you of the causality of LDL on CVD, I’m not sure what is.
I (Layne) say this as someone who, for many years, believed the same thing Paul believed. In 2004 when I got to graduate school, I remember reading quite a bit about HDL, TAGs, and LDL. My conclusion was that LDL probably mattered, but only in the context of reduced HDL and increased TAGs. This was also similar to my Ph.D. advisor’s stance on the topic. It wasn’t until YEARS later, after I graduated when I began reading some of the new research, that I realized I was WRONG. It even made me change the way I eat since I’m someone who runs with a naturally higher LDL (~170mg/dl if I don’t make dietary adjustments). I WISH what Paul is saying was true. I believed it for a long time, and it formed my bias for a LONG (>10 years) time. But my feelings and bias are not more important than HARD DATA. This is why we wrote this article, because not only is what Paul is saying incorrect, it’s also dangerous.
Paul also says PUFAs increased the rates of cancer, but that is not what the experiment demonstrated and was not a conclusion of the researchers. Remember, this is a SINGLE RCT. I can find a single study to support nearly ANYTHING I want, and that’s precisely what Paul is doing. In a meta-analysis of 49 RCTs with over 24,000 participants, replacing SFA with PUFA did not increase mortality and did slightly lower the incidence of CVD. [225] Now, you might be thinking, “Ah-ha! PUFA only slightly lowered CVD risk, so what’s the point?” Remember that this is a lifetime exposure risk problem, and many of these trials were only a year or two. Will lowering your LDL for a year or two drastically reduce your risk? Probably not, just like investing $2000 every year at 8% interest vs. 6% interest for a few years won’t get you a big difference in return on your investment, but investing $2000 every year for 30+ years absolutely will.
If you are 80 years and run modestly high LDL, would switching out to PUFA from SFA make a big difference? Unlikely unless you live to 100. But if you are 50 and start making changes, it could have a significant impact by the time you are in your 70s or 80s. Likewise, if you are in your 20s or 30s, it could make a considerable difference based on the MR and statin trial data. Paul’s statement that PUFA increases cancer compared to SFA is absolute NONSENSE. A huge systematic review examining the studies on the amount of dietary fat and dietary fat types on various cancers found very few associations between any kind of dietary fat and any kind of cancer. There were a few exceptions with pooled results showing some association of SFA with pancreatic cancer but in none of the cases were higher PUFA intakes associated with increases in cancer incidence once the results from all studies were pooled. There were a few cancer types where PUFA had a significant protective effect, with a particularly strong protective effect on gastric cancer. [226] Please keep in mind what Paul is doing. He is finding single, isolated studies to support his points. This is not how science works; science looks at the TOTALITY of data. In this case, his statements aren’t even backed by the data from the study he is citing.
02:07:45 Claim: Joe says if eating all meat is bad for you, why does he feel so good? Paul responds by agreeing with him.
Reality: Plenty of people feel great right up until the day they have a heart attack or get diagnosed with cancer. You can’t “feel” LDL damaging your arteries, and you can’t “feel” atherosclerosis. When it comes to feelings, there’s not much I can do because feelings aren’t data. People believe what they want to believe.
02:14:57 Claim: “If you look at the medical literature, there’s no evidence fiber improves constipation.”
Reality: Categorically untrue. [227][228][229] Is it a huge effect? No. Is it going to take someone who struggles with constipation and be the end-all solution? No. But it does increase bowel movement frequency. There is a single case report series that Paul loves to cherry-pick, which followed people who reduced fiber intake and reported improvement in constipation. [230] Paul said this was a control trial where they put people on different fiber intakes, but it wasn’t a control trial. They were asked to go on a no fiber diet for 2 weeks then add back fiber to a level they felt comfortable with. This was 63 people, and there was NO control group. Compare this to the systematic reviews of thousands of data points. Now, are there isolated cases and individuals where stopping or reducing fiber might help with constipation? It appears there are, yes. Does that mean fiber is useless, and we should tell people to eat less of it? Absolutely NOT. This is like saying no one should consume dairy because a subset of the population is lactose intolerant, even though dairy also has many health benefits (high-quality protein, calcium, vitamin D, etc.).
It’s important to understand the difference between cherry-picking a single data point or study vs. looking at the totality of evidence. If you want to seek out a study that validates what you already believe to be true, you can almost certainly find SOMETHING that will support it. That is why looking at isolated studies is NOT rigorous science. Looking at the totality of evidence is. Check out this forest plot of cigarette smoking and adenocarcinoma studies. [231] The studies with the squares to the right of the “1” line indicate a harmful effect. The further to the right they are, the more harm is shown in the study. The confidence intervals are also included. To avoid getting into a discussion of significance, just understand that the wider the interval, the more variability was seen between subjects in the studies. Also, the larger the square, the more subjects in the study. At the very bottom, you will see a diamond. The diamond represents the summation of all the studies.
The summation is a 4.21 increase in RR (relative risk), which is enormous. There aren’t very many people who would dispute that smoking is bad for cancer, but check out the two studies to the LEFT of the centerline, indicating a potentially PROTECTIVE effect of smoking on adenocarcinoma. If I wanted to take a position that smoking wasn’t bad, I could cite those two studies and say, “Look, this shows smoking doesn’t cause adenocarcinoma and might even protect you against it!” But that neglects the OVERALL body of evidence showing a substantial negative effect of smoking (shoutout to Nick Hierbert @the_nutrivore for his assistance with this).
Figure: Forest plot of current smoking of any product and adeno.
Table presents the results of a main meta-analysis for adeno based on 44 relative risk (RR) and 95% confidence interval (CI) estimates for current smoking of any product (or cigarettes if any product not available). The individual study estimates are shown numerically and graphically on a logarithmic scale. The studies are sorted in order of sex within study reference (REF) within start year of study (START) within continent (CONT). In the graphical representation individual RRs are indicated by a solid square, with the area of the square proportional to the weight (inverse-variance of log RR). Arrows indicate where the CI extends outside the range allocated. Also shown are the combined random-effect estimates. These are represented by a diamond of standard height, with the width indicating the 95% CI.
This is exactly what Paul is doing with many of his claims. He finds isolated studies like the Minnesota Coronary Experiment or this 63 person case study series on fiber and constipation to use as “evidence” that his claims are correct. But they are not accurate based on the OVERALL BODY OF EVIDENCE. That said, the effect of fiber on constipation is not as powerful as smoking is on adenocarcinomas. Still, I felt it was important to use an extreme example of how cherry-picking works. Again, fiber does not have a huge effect overall, but it does improve some aspects of constipation.
Constipation, however, is not the main reason you should eat a diet rich in fiber. There are a ton of health benefits to high fiber consumption. There is strong evidence that fiber can reduce incidence and mortality of heart disease and cancer. [232][233][234][235][236] A recent umbrella review of 31 meta-analyses (we are talking millions of data points) performed on this topic showed consistently favorable outcomes when comparing the highest intake of fiber vs. the lowest intake. In heart disease, this is likely due to soluble fiber’s ability to lower LDL cholesterol by around 10-14mg/dl, which should correspond to about a 20-25% risk reduction for CVD based on the previous graph regarding the linear dose relationship between LDL & CVD. Interestingly, this predicted risk reduction is very similar to what is observed in the outcome data of the literature. [237]
In cancer, fiber intake appears to have the most potent effect at reducing colorectal cancer while also having a possible preventative effect on esophageal, gastric, pancreatic, rectal, ovarian, and breast cancer. [238][239][240]
Forest plot of prospective cohort studies of (A) cardiovascular disease mortality, (B) coronary heart disease mortality and (C)all-cancer mortality for the highest versus lowest category of dietary fibre intake, using a random-effects model. CI: confidence interval;F: females; M: males; RR: relative risk.
Not only is this effect very consistent amongst various studies with few exceptions but that the results are also consistent within the meta-analyses of these studies. It’s not like there is a large body of studies that don’t show this effect, the vast majority DO show this effect, which is why it is so consistent amongst the systematic reviews and meta-analysis (the gold standard of scientific research) Since these meta-analysis do not fit with the bias of people like Paul, he would probably default to saying that this is simply “healthy user bias,” meaning that it’s not the fiber that’s causing these effects, more so that people who eat high fiber are simply more likely to be more healthy overall. While healthy user bias is a real thing, using it as a shield against any data you simply don’t like or agree with is weak. Further, healthy user bias might be a valid criticism of specific epidemiological studies. Still, when we observe the effect REPEATEDLY throughout DOZENS of META-ANALYSES that contain many studies and millions of data points, while also having an established mechanism for how this dietary component may have a favorable effect, then we can have a lot of confidence that this is not just “healthy user bias.” Does eating enough fiber mean you won’t get cancer? No. Does eating enough fiber mean you won’t get colon cancer? No. It just reduces your risk by probably about ~20% or so based on the studies. If you eat a Carnivore Diet does that mean you WILL get colon cancer? No. But you simply increase your risk. Just like smoking doesn’t mean you will die of lung cancer or CVD, but it increases your risk.
It’s also important to note that if you are going to eat a diet with a high meat intake, it’s probably IMPORTANT that you also consume a high amount of fruits and vegetables. People who eat diets high in meat (mostly red and processed meat) tend to have higher cancer rates. [241][242][243] Vegan zealots have used this information to claim that meat causes cancer, but this is confounded by the fact that people who eat more meat also tend to eat fewer fruits and vegetables. A recent study sought to reconcile these variables by examining various intakes of red meat and processed meat (low, medium, and high) with varying intakes of fruits and vegetables (low, medium, and high). The researchers found an association of red meat with all cancer when fruit and vegetable consumption was low. When it was high, there was no association of red meat with cancer, even at the highest red meat intake. [244] The metric used to assess the relationship between meat, fruits, and vegetables was what’s called a “hazard ratio (HR).” An HR of 1 means there is the same risk in the group you are assessing compared to the control group. For this study, they used the highest intake of fruits and vegetables and the lowest meat intake as the control. As you can see from the image below taken from my Instagram account, the HR for high meat consumption plus high fruit and vegetable consumption was lower (though not significantly) than the control. Interestingly, at both moderate and high levels of meat consumption, there was a linear decrease in HR based on increasing fruit and vegetable consumption.
This indicates that meat consumption might not be the issue regarding cancer, but rather the fact that people who eat a lot of meat don’t eat many fruits and vegetables. This study highlights something I’ve been saying for a while: I don’t think meat consumption necessarily causes cancer risk, rather that people who eat a lot of meat end up displacing other nutrients that have a protective effect on cancer, like fruits and vegetables. So if you want to have a high intake of meat, fine, but you better also have a high intake of fruits and vegetables.
It is important to note that even at high fruit and vegetable intake, processed meat still retained an increased HR (1.66).
I realize I’m arguing a point Paul has not made about plants and fiber in this interview, and I don’t want to strawman him. However, he has alluded to this in previous interviews as well as in a debate with me. I just find it interesting that he will cling to tenuous links between mechanistic data that is NOT supported by outcome data when it comes to things like PUFAs, but will fail to acknowledge the data on fiber (as well as saturated fat & LDL) that demonstrates actual OUTCOMES and is also supported by stronger mechanistic data. It’s one of the many examples of Paul invoking a specific line of logic when it suits his bias, then discarding it when it doesn’t.
02:17:41 No Claim: but Paul mentions he was a raw vegan for 7 months. Just pointing out that Paul is likely an extremist. He went from one extreme diet (raw vegan) to another extreme diet (carnivore). This is not how experts make changes.
02:21:57 Claim: Joe asks Paul what he would say to people who don’t have an ideology who want to do what’s best for their heart (when discussing people who have had heart surgery or transplants) to which Paul replies, “have them eat like their ancestors, eat like the Hadza…”
Reality: This is funny for many reasons.
- Joe saying, “people without ideology” when Paul AND Joe have very clearly invested themselves in Carnivore ideology.
- This idea we should eat like our ancestors because that’s what is best is an appeal to nature fallacy, but moreover, as we already discussed, our ancestors ate a pretty diverse diet. One of the studies on ancestral diet diversity states, “the dietary capabilities of the earliest hominids changed dramatically, leaving them well suited for life in a variety of habitats and able to cope with significant changes in resource availability associated with long-term and short-term climatic fluctuations.” [246] According to Paul, they mostly just ate meat. If that were true, why do we have such dissimilar gastrointestinal digestive biology compared to a carnivore’s, like felines who eat meat exclusively in the wild but have extremely short GI tracts with much different morphology compared to humans? [247][248] Interestingly, the diets of our closest living animal relative, chimpanzees, rarely eat meat, and while they eat an extremely diverse diet, it’s predominantly plant-based. [249] So Paul wants us to believe that we went from being mostly plant-eaters with a very diverse diet to almost exclusively meat-based? It doesn’t make logical sense, and it’s simply not supported by the anthropological data.
- Paul said we should eat like the Hadza. Interestingly, Paul has said numerous times that we should eat more like our ancestors (the Hadza are a modern hunter-gatherer tribe that hasn’t really been touched by modern civilization) but has also said that he thinks saturated fat isn’t bad for us and LDL isn’t the cause of heart disease. Funny enough, hunter-gatherer tribes like the Hadza do have low rates of heart disease, but they also have some of the lowest LDL levels, eat paltry amounts of saturated fat, and eat high amounts of fruits and vegetables. [250][251] The Hadza get over 85% of their calories from fruit and vegetables during various times of the year. The LDL le.els of hunter-gatherer tribes average between 50-75mg/dl, INCLUDING THE HADZA! [252][253][254] That is EXTREMELY LOW. Paul said his LDL was over 300mg/dl (I believe he’s even said it’s been as high as 500mg/dl during another interview), but he thinks it’s ok because his HDL is also high. Ironically, the Hadza have low HDL levels (~35mg/dl)but don’t get heart disease, highlighting once again that LDL is more important. I agree with Paul that we probably should eat more like our ancestors. The catch is that the diet Paul advocates for and consumes is NOT WHAT OUR ANCESTORS LIKELY ATE, at least not most of them. Still, some tribes ate more meat and had higher LDL than others. Some Eskimo tribes have LDL levels above 150mg/dl but have much higher heart disease rates than other hunter-gatherer tribes. [256][257][258][259][260][261] The pre-text of Paul’s entire philosophy on the Carnivore Diet isn’t even supported by the evidence.
02:24:00 Claim: Vegan diets become an identity, a kind of person
Reality: All diet tribes are like this, carnivore included. Notice how people like Kevin and I do not have a particular diet listed in any of our bios anywhere. If you peruse Paul’s Instagram, you will notice his username is “@carnivoremd.” How is that not an identity? Imagine Paul admitting he’s wrong on any of this? He would have to change all his social media handles and his identity because he literally identifies himself as his diet. The fact that he doesn’t see that what he does is the same thing that vegan physician extremists like Dr. Michael Gregor and Dr. Garth Davis do (logical fallacies, cherry-picking, refusing to acknowledge contrary data) is a testament to how far into his belief system he is.
Next, Joe and Paul discuss the merits of hunting (hey, I love to fish, so no hate). The interesting thing is they talk about how much they love how it makes them feel and how eating the meat makes them feel. Here’s what I don’t understand. Joe said he was either going to be a vegetarian or a hunter, and after killing his first animal and eating it, he said, “This is what I’m going to do.” Ok, that is great. But why do Paul or Joe need to justify their choices regarding enjoying hunting and eating meat with science? If you just like it, say you like it. This is the same thing that extreme vegans do. They decide that veganism is what they want to do. Then many of them retroactively justify their choice not by saying, “I prefer this,” but rather by doing mental gymnastics and fuckery with the scientific literature to justify and validate THEIR CHOICE. This is precisely what Paul, and to a lesser extent, Joe, is doing. I love to fish, but if there were a massive amount of data that said eating fish was terrible for me, I wouldn’t try to cherry-pick and do mental gymnastics, I would simply say, “I just like doing this, and I understand the possible consequences.”
02:49:00 Claim: Grass-fed/grass-finished beef will have less “bad stuff” in it than grass-fed/grain-finished beef.
Reality: There are some differences in total fat content and fatty acid content between these two types of beef; whether or not that would make an impact on long term health is difficult to know. [262] Paul doesn’t get specific with the “bad stuff,” but he does mention glyphosate, which is commonly known as Roundup, the weed killer sprayed on many farm grounds. While this sounds horrible and scary, and there is some epidemiology to support high intakes of glyphosate on a few different cancers, please keep in mind that this is the same epidemiology data that Paul calls “garbage.” [263] Perhaps grass-finished is better than grain-finished in various ways, and perhaps glyphosate is a health risk (remember that the dosage makes the poison, and it means it would need to wind up in our food in high amounts), but thus far, it’s only correlation data. Paul loves to say that it’s just “healthy user bias” when he disagrees with the data on fiber, then why can’t we apply that same logic to his claim here and say that this is just unhealthy user bias? That is, people who eat higher amounts of grain-finished beef (less expensive) are probably eating more unhealthy overall and more likely to develop these cancers. I don’t know this to be true, but I figure if Paul can speculate about why certain epidemiological studies are “garbage,” why can’t I? Once more, this highlights how Paul invokes certain logic when it suits him but discards that same logic when it no longer does.
02:49:20 Claim: There’s not a big difference between grass-fed vs. grain-fed on the nutritional content of the beef.
Reality: Just pointing out that I agree with Paul on this and want to give him credit where credit is due.
02:51:30 Claim: There’s something about eating grass-fed meat that is rewarding to your body, and you feel great, says Joe.
Reality: That’s probably true, but only because Joe believes it to be true. MANY studies demonstrate the power of placebo is similar to drugs. [264][265][266][267] When people hear “placebo effect,” they tend to think of it as fabricating how you feel. They think I’m saying that they aren’t experiencing what they claim, and it’s all in their head. What I’m saying is that placebo and the power of suggestion have POWERFUL effects on brain chemistry and can cause PHYSIOLOGICAL CHANGES to our bodies. [268][269][270] I’m not saying that this is all in Joe’s head. What I am saying is that it doesn’t necessarily apply to anyone else other than Joe. He believes that meat will make him feel good because that is part of his belief system, so when he eats it, he probably does feel good. But that doesn’t mean that meat has a real, measurable effect other than placebo.
02:54:41 Claim: If you eat enough meat (1lb), you don’t need to supplement with creatine. There is about 5g of creatine in 1lb of meat.
Reality: I’m not sure where he’s getting this data from. Based on what I’ve seen, there is about 22.5mmol creatine per kg of meat. Unless my stoichiometry is rusty, that equates to about 2.95g/kg, but 50% of that is converted to creatinine during cooking and thus is a waste product rather than a valuable bioactive compound. [271][272] That means the actual creatine content is around ~1.5g creatine/kg cooked beef. To achieve 5g of creatine per day would require approximate consumption of approximately 3.4kg (7lbs) of cooked beef per day. I guess some Carnivores might get that, but at 3.4kg, even your leanest top sirloin is about 165 kcal/100g, and therefore at MINIMUM, you’d be eating ~5600 calories per day from beef to hit 5g of creatine. This is kind of like the “peanut butter sandwich has as much protein as 3 oz of steak or 3 eggs” statement from The Game Changers film. Sure, you can get 20g of protein from a peanut butter sandwich, but you’re going to get significantly MORE calories than if you ate a typical protein source. Similarly, if you are pitching the Carnivore Diet as a way not to have to worry about creatine supplementation, I guess it’s possible, but not very practical at all.
03:00:30 Claim (summarized): I’m not against plants as drugs; I’m against them as food.
Reality: Paul talks about medical marijuana and psilocybin as potential therapeutics, and I am not discounting the possibility of that, but if you look at the evidence of their efficacy, it’s significantly less, and there is way less research than that showing that plants are healthful as part of our diet. At this point, it’s incredible how Paul can invoke a line of logic and then discard it so quickly.
Summary
This was very painful to listen to. Paul has the benefit of knowing a lot of medical jargon and has read many of the studies he is citing. The problem is he ONLY talks about those studies and NEGLECTS entire portions of scientific literature. Or, as he demonstrated repeatedly, he will flippantly use (or discard) logic at his discretion. He also will use epidemiology to support his arguments when it suits him but then dismiss it as “garbage” when it doesn’t fit his bias. That is not good science. That is not rigorous science. While I am happy to hear that Paul no longer thinks that carbohydrates, in general, are making us fat and sick, he still clings to extremely weak, cherry-picked data to support the majority of his positions.
I am not against being a contrarian. It is crucial to challenge ideas. But in the words of Christopher Hitchens, “Extraordinary claims require extraordinary evidence.” Cherry-picking random epidemiology and RCTs that fit your bias is not extraordinary evidence. If you like eating meat, fine. Meat can be part of a healthy diet, but so can plants.
References
- “Heterocyclic Amines: Mutagens/carcinogens … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/15072585/. Accessed 3 Nov. 2020.
- “Trimethylamine N-oxide, a gut microbiota-dependent … – NCBI.” 20 Nov. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6245753/. Accessed 3 Nov. 2020.
- “The Multifaceted Role of Heme in Cancer – NCBI – NIH.” 15 Jan. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6974621/. Accessed 3 Nov. 2020.
- “Vegetarian, vegan diets and multiple health outcomes: A ….” 22 Nov. 2017, https://pubmed.ncbi.nlm.nih.gov/26853923/. Accessed 3 Nov. 2020.
- “Healthy Plant-Based Diets Are Associated with Lower Risk of ….” 11 Apr. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6669955/. Accessed 3 Nov. 2020.
- “Antiproliferative Effect of Indole Phytoalexins – NCBI.” 26 Nov. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6274154/. Accessed 3 Nov. 2020.
- “Differences in food consumption between patients with … – NCBI.” 30 Jun. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7327046/. Accessed 3 Nov. 2020.
- “Phytoestrogens and Their Health Effect – NCBI – NIH.” 14 Feb. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6390141/. Accessed 4 Nov. 2020.
- “Soy protein supplementation is not androgenic or estrogenic ….” 24 Jul. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6057888/. Accessed 4 Nov. 2020.
- “Clinical studies show no effects of soy protein or isoflavones ….” 12 Jun. 2009, https://pubmed.ncbi.nlm.nih.gov/19524224/. Accessed 4 Nov. 2020.
- “Exercise intensity and its effects on thyroid hormones – PubMed.” https://pubmed.ncbi.nlm.nih.gov/16380698/. Accessed 4 Nov. 2020.
- “Thyroid hormone responses to endurance exercise – PubMed.” https://pubmed.ncbi.nlm.nih.gov/17402388/. Accessed 4 Nov. 2020.
- “Effect of Exercise on Serum Sex Hormones in Men: A 12 ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3040039/. Accessed 4 Nov. 2020.
- “Gender differences in exercise-induced changes in sex ….” https://pubmed.ncbi.nlm.nih.gov/11249932/. Accessed 4 Nov. 2020.
- “Exercise-induced vomiting – NCBI – NIH.” 30 Dec. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4027831/. Accessed 4 Nov. 2020.
- “Runner’s diarrhea: what is it, what causes it, and how can it be ….” https://pubmed.ncbi.nlm.nih.gov/27798441/. Accessed 4 Nov. 2020.
- “Rhabdomyolysis – StatPearls – NCBI Bookshelf.” 10 Jul. 2020, https://www.ncbi.nlm.nih.gov/books/NBK448168/. Accessed 4 Nov. 2020.
- “Influence of Acute Exercise on DNA Repair and PARP … – NCBI.” 19 Jun. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6628277/. Accessed 4 Nov. 2020.
- “Sunlight damage to cellular DNA: Focus on … – PubMed.” 18 Jan. 2017, https://pubmed.ncbi.nlm.nih.gov/28109890/. Accessed 4 Nov. 2020.
- “Clinical Effects of Regular Dry Sauna Bathing: A Systematic ….” 24 Apr. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5941775/. Accessed 4 Nov. 2020.
- “Benefits and risks of sauna bathing – PubMed.” https://pubmed.ncbi.nlm.nih.gov/11165553/. Accessed 4 Nov. 2020.
- “Mechanisms of atrial fibrillation in athletes: what we know and ….” 6 Feb. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5818379/. Accessed 4 Nov. 2020.
- “Resistance training alone reduces systolic and diastolic blood ….” 3 Aug. 2017, https://pubmed.ncbi.nlm.nih.gov/28769100/. Accessed 4 Nov. 2020.
- “Inflammatory Effects of High and Moderate Intensity Exercise ….” 9 Jan. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6962351/. Accessed 4 Nov. 2020.
- “Exercise-Induced Oxidative Stress and the Effects of … – NCBI.” 5 Sep. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6162669/. Accessed 4 Nov. 2020.
- “Exercise and circulating cortisol levels: the intensity threshold ….” https://pubmed.ncbi.nlm.nih.gov/18787373/. Accessed 4 Nov. 2020.
- “Exercise and the Heart: Risks, Benefits, and … – NCBI.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3116747/. Accessed 4 Nov. 2020.
- “Physical Activity and Onset of Acute Ischemic Stroke – NCBI.” 15 Dec. 2010, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4192041/. Accessed 4 Nov. 2020.
- “Induction of Phase 2 Antioxidant Enzymes by Broccoli … – NCBI.” 24 Jan. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3264924/. Accessed 4 Nov. 2020.
- “Sulforaphane and Other Nutrigenomic Nrf2 … – NCBI – NIH.” 6 Jan. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4736808/. Accessed 4 Nov. 2020.
- “Brassica-Derived Plant Bioactives as Modulators of … – NCBI.” 1 Sep. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5618539/. Accessed 4 Nov. 2020.
- “Dietary Regulation of Keap1/Nrf2/ARE Pathway – NCBI – NIH.” 19 Sep. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4179188/. Accessed 4 Nov. 2020.
- “Caveats for the Good and Bad of Dietary Red Meat – NCBI – NIH.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6912709/. Accessed 4 Nov. 2020.
- “A red meat-derived glycan promotes inflammation and cancer ….” 29 Dec. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4299224/. Accessed 4 Nov. 2020.
- “Sulforaphane Protects against Cardiovascular … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/26583056/. Accessed 4 Nov. 2020.
- “Sulforaphane as a Potential Protective Phytochemical against ….” 25 Jul. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3745957/. Accessed 4 Nov. 2020.
- “The role of Sulforaphane in cancer chemoprevention and ….” 23 Jul. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5842175/. Accessed 4 Nov. 2020.
- “Full article: Fruits, vegetables, and health: A comprehensive ….” 3 Jul. 2019, https://www.tandfonline.com/doi/full/10.1080/10408398.2019.1632258. Accessed 4 Nov. 2020.
- “Heme iron from meat and risk of adenocarcinoma … – NCBI – NIH.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261306/. Accessed 4 Nov. 2020.
- “Heme iron from meat and risk of colorectal cancer: a meta ….” https://pubmed.ncbi.nlm.nih.gov/21209396/. Accessed 4 Nov. 2020.
- “Heme, an Essential Nutrient from Dietary Proteins, Critically ….” 13 Mar. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3967179/. Accessed 4 Nov. 2020.
- “Effect of fruit and vegetable intake on oxidative … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/22088966/. Accessed 4 Nov. 2020.
- “The 6-a-day study: effects of fruit and vegetables on markers ….” https://pubmed.ncbi.nlm.nih.gov/15159237/. Accessed 4 Nov. 2020.
- “Effects of fruit and vegetable consumption on inflammatory ….” 21 Jun. 2018, https://academic.oup.com/ajcn/article/108/1/136/5042153. Accessed 4 Nov. 2020.
- “A hydroxyl group of flavonoids affects oral anti-inflammatory ….” https://pubmed.ncbi.nlm.nih.gov/14745173/. Accessed 4 Nov. 2020.
- “Vitamin C and Neutrophil Function: Findings from … – NCBI.” 4 Sep. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770220/. Accessed 4 Nov. 2020.
- “A new recommended dietary allowance of vitamin C for ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC55540/. Accessed 4 Nov. 2020.
- “Vitamin C for preventing and treating the common … – PubMed.” 31 Jan. 2013, https://pubmed.ncbi.nlm.nih.gov/23440782/. Accessed 4 Nov. 2020.
- “Vitamin C in the Prevention and Treatment of the Common Cold.” 9 Feb. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6124957/. Accessed 4 Nov. 2020.
- “Extra Dose of Vitamin C Based on a Daily Supplementation ….” 5 Jul. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6057395/. Accessed 4 Nov. 2020
- “Paul Saladino, MD on Twitter: “Lower LDL levels in patients ….” 19 Mar. 2020, https://twitter.com/carnivoremd/status/1240684108860125185?lang=en. Accessed 4 Nov. 2020.
- “Removing the Meat Subsidy: Our Cognitive Dissonance ….” 11 Feb. 2020, https://jia.sipa.columbia.edu/removing-meat-subsidy-our-cognitive-dissonance-around-animal-agriculture. Accessed 20 Oct. 2020.
- “Animal Agriculture Subsidies Threaten Our Planet.” 19 Dec. 2016, https://cleantechnica.com/2016/12/19/animal-agriculture-subsidies-threaten-planet/. Accessed 20 Oct. 2020.
- “Agricultural policies, food and public health – NCBI.” 10 Dec. 2010, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3024136/. Accessed 20 Oct. 2020.
- “Does current food production meet global nutritional … – NCBI.” 23 Oct. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6198966/. Accessed 6 Nov. 2020.
- “The Transformation of US Livestock Agriculture – USDA ERS.” https://www.ers.usda.gov/webdocs/publications/44292/10992_eib43.pdf?v=0. Accessed 6 Nov. 2020.
- “Nationwide shift to grass-fed beef requires larger cattle ….” 25 Jul. 2018, https://iopscience.iop.org/article/10.1088/1748-9326/aad401. Accessed 20 Oct. 2020.
- “Is the Grass Always Greener? Comparing the … – NCBI.” 10 Apr. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4494320/. Accessed 20 Oct. 2020.
- “Environmental impacts of beef production: Review … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/26117397/. Accessed 20 Oct. 2020.
- “Ethan Weiss on Twitter: “1/ Today is Yom Kippur. Many Jewish ….” 28 Sep. 2020, https://twitter.com/ethanjweiss/status/1310595463452614656. Accessed 20 Oct. 2020.
- “JAMA Internal Medicine – JAMA Network.” 28 Sep. 2020, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2771095. Accessed 20 Oct. 2020.
- “Intermittent versus continuous energy restriction on … – PubMed.” 24 Dec. 2018, https://pubmed.ncbi.nlm.nih.gov/30583725/. Accessed 20 Oct. 2020.
- “Time-Restricted Eating Doesn’t Work for Weight Loss | UC San ….” 28 Sep. 2020, https://www.ucsf.edu/news/2020/09/418611/time-restricted-eating-doesnt-work-weight-loss. Accessed 20 Oct. 2020.
- “Obesity Energetics: Body Weight Regulation and the … – NCBI.” 11 Feb. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5568065/. Accessed 20 Oct. 2020.
- “Comparison of dietary macronutrient patterns of 14 … – The BMJ.” 1 Apr. 2020, https://www.bmj.com/content/369/bmj.m696. Accessed 20 Oct. 2020.
- “The effect of fasting or calorie restriction on autophagy ….” 30 Aug. 2018, https://pubmed.ncbi.nlm.nih.gov/30172870/. Accessed 21 Oct. 2020.
- “The Effects of Calorie Restriction on Autophagy: Role … – NCBI.” 2 Dec. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6950580/. Accessed 21 Oct. 2020.
- “Caloric restriction and resveratrol promote longevity … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/21364612/. Accessed 21 Oct. 2020
- “The effect of fasting or calorie restriction on autophagy ….” 30 Aug. 2018, https://pubmed.ncbi.nlm.nih.gov/30172870/. Accessed 21 Oct. 2020.
- “Plant-animal subsistence ratios and macronutrient energy ….” https://pubmed.ncbi.nlm.nih.gov/10702160/. Accessed 21 Oct. 2020.
- “Evolutionary Adaptations to Dietary Changes – NCBI – NIH.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4163920/. Accessed 21 Oct. 2020.
- “Honey, Hadza, hunter-gatherers, and human evolution.” https://pubmed.ncbi.nlm.nih.gov/24746602/. Accessed 21 Oct. 2020.
- “Nutrition, modernity and the archaeological record: Coastal ….” https://www.sciencedirect.com/science/article/abs/pii/S0047248414002073. Accessed 21 Oct. 2020.
- “How to Really Eat Like a Hunter-Gatherer: Why the Paleo Diet ….” 3 Jun. 2013, https://www.scientificamerican.com/article/why-paleo-diet-half-baked-how-hunter-gatherer-really-eat/. Accessed 21 Oct. 2020.
- “Atherosclerosis across 4000 years of human history … – PubMed.” 6 Apr. 2013, https://pubmed.ncbi.nlm.nih.gov/23489753/. Accessed 21 Oct. 2020.
- “Dairy Intake Enhances Body Weight and Composition … – NCBI.” 1 Jul. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4963870/” target=”_blank. Accessed 21 Oct. 2020.
- “Effect of dairy consumption on weight and body composition in ….” https://pubmed.ncbi.nlm.nih.gov/22249225/. Accessed 21 Oct. 2020
- “Normal/high-fat milk consumption is associated with higher ….” 2 Feb. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5796600/. Accessed 21 Oct. 2020.
- “Whole-grain intake and cancer: an expanded review and meta ….” https://pubmed.ncbi.nlm.nih.gov/9589426/. Accessed 21 Oct. 2020.
- “Whole grain intake and cardiovascular disease: a … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/17449231/. Accessed 21 Oct. 2020.
- “Whole Grain Intake and Mortality From All Causes ….” 14 Jun. 2016, https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.115.021101. Accessed 21 Oct. 2020
- “‘Going Vegan Cured My Autoimmune Disease” – Body + Soul.” 24 Jul. 2018, https://www.bodyandsoul.com.au/health/womens-health/going-vegan-cured-my-autoimmune-disease/news-story/8adb564394c8c49f15aa3879aaae6494. Accessed 21 Oct. 2020.
- “I went vegan and it cured my autoimmune disease.” 24 Jul. 2018, https://nypost.com/2018/07/24/i-went-vegan-and-it-cured-my-autoimmune-disease/. Accessed 21 Oct. 2020.
- “A Vegan Diet Helped Me Treat My Autoimmune Disease.” 5 Jun. 2020, https://thebeet.com/a-vegan-diet-helped-me-treat-my-autoimmune-disease-says-nour-danno/. Accessed 21 Oct. 2020.
- “Can a Plant-Based Diet Help With Autoimmune Disease ….” 27 Mar. 2020, https://www.livekindly.co/plant-based-diet-autoimmune-disease/. Accessed 21 Oct. 2020.
- “A Whole Food, Plant-Based Approach to Autoimmune ….” 3 Apr. 2020, https://nutritionstudies.org/a-whole-food-plant-based-approach-to-autoimmune-diseases-in-4-steps/. Accessed 21 Oct. 2020.
- “Immunomodulatory Effects of Diet and Nutrients in Systemic ….” 22 Jul. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7387408/. Accessed 21 Oct. 2020.
- “Dietary intake of soluble fiber and risk of islet autoimmunity by ….” 8 Jul. 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4515865/. Accessed 21 Oct. 2020.
- “Dietary non-fermentable fiber prevents autoimmune … – NCBI.” 11 Jul. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6041322/. Accessed 21 Oct. 2020.
- “The Role of Dietary Fiber in Rheumatoid Arthritis Patients: A ….” 7 Oct. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6836071/. Accessed 21 Oct. 2020.
- “Intake frequency of vegetables or seafoods negatively … – NCBI.” 13 Feb. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7018088/. Accessed 21 Oct. 2020
- “Immunomodulatory Effects of Diet and Nutrients in Systemic ….” 22 Jul. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7387408/. Accessed 21 Oct. 2020.
- “Nutrition Interventions in Rheumatoid Arthritis: The Potential ….” 10 Sep. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6746966/. Accessed 21 Oct. 2020.
- “The Influence of Dietary Fatty Acids on Immune Responses.” 6 Dec. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6950146/. Accessed 21 Oct. 2020
- “Therapeutic Potential of ω-3 Polyunsaturated Fatty Acids in ….” 27 Sep. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6776881/. Accessed 21 Oct. 2020.
- “Polyunsaturated fatty acids, inflammation, and immunity.” https://pubmed.ncbi.nlm.nih.gov/11724453/. Accessed 21 Oct. 2020.
- “Fatty acids, the immune response, and autoimmunity: a ….” https://pubmed.ncbi.nlm.nih.gov/12848277/. Accessed 21 Oct. 2020.
- “Saturated fat, especially long chain… – Paul Saladino MD ….” 20 Jun. 2020, https://www.facebook.com/carnivoreMD/posts/2897774587016466. Accessed 21 Oct. 2020.
- “How We’ve Been Lied to About Saturated Fat – YouTube.” 24 Jun. 2020, https://www.youtube.com/watch?v=iUtlCApYm_I. Accessed 21 Oct. 2020.
- “How Linoleic Acid is making you fat and Stearic Acid might ….” https://carnivoremd.com/how-linoleic-acid-is-making-you-fat-and-stearic-acid-might-just-be-the-remedy-with-brad-marshall-aka-the-croissant-diet-guy/. Accessed 21 Oct. 2020.
- “Role of “Western diet” in inflammatory autoimmune diseases.” https://pubmed.ncbi.nlm.nih.gov/24338487/. Accessed 21 Oct. 2020.
- “Life Span Is Prolonged in Food-Restricted Autoimmune-Prone ….” https://academic.oup.com/jn/article/131/10/2753/4686521. Accessed 21 Oct. 2020.
- “Diet, microbiota and autoimmune diseases – VIVO.” http://vivo.med.cornell.edu/display/pubid84899538713. Accessed 21 Oct. 2020.
- “Nutrient Modulation of Autoimmune Disease – Wiley Online ….” http://onlinelibrary.wiley.com/doi/10.1111/j.1749-6632.1990.tb00148.x/pdf. Accessed 21 Oct. 2020.
- “The neuroscience of placebo effects: connecting context ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6013051/. Accessed 21 Oct. 2020
- “How Placebos Change the Patient’s Brain – NCBI.” 30 Jun. 2010, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3055515/. Accessed 21 Oct. 2020
- “Mechanisms and Clinical Implications of the Placebo Effect: Is ….” 26 Oct. 2010, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3130981/. Accessed 21 Oct. 2020.
- (n.d.). The Hadza: Hunter–Gatherers of Tanzania – ResearchGate. Retrieved November 5, 2020, from https://www.researchgate.net/publication/285982929_The_Hadza_Hunter-Gatherers_of_Tanzania
- (n.d.). Effects of pure sugar vs. mixed starch fructose loads … – PubMed. Retrieved November 5, 2020, from https://pubmed.ncbi.nlm.nih.gov/1799283/
- (n.d.). Effects of fructose and glucose preloads on … – PubMed. Retrieved November 5, 2020, from https://pubmed.ncbi.nlm.nih.gov/3592650/
- (n.d.). Comparison of oral and gastric administration of … – PubMed. Retrieved November 5, 2020, from https://pubmed.ncbi.nlm.nih.gov/11791150/
- (n.d.). The Hadza: Hunter–Gatherers of Tanzania – ResearchGate. Retrieved November 5, 2020, from https://www.researchgate.net/publication/285982929_The_Hadza_Hunter-Gatherers_of_Tanzania
- (n.d.). Hunter‐gatherers as models in public health – Wiley Online …. Retrieved November 5, 2020, from https://onlinelibrary.wiley.com/doi/full/10.1111/obr.12785
- (n.d.). Intensive Lifestyle Changes for Reversal of Coronary Heart …. Retrieved November 5, 2020, from https://www.ornish.com/app/uploads/Intensive-lifestyle-changes-for-reversal-of-coronary-heart-disease1.pdf
- Lee, R. B., & DeVore, I. (Eds.). (1973). Man the hunter. Chicago, IL: Aldine Publishing Company.
From Woodburn’s section - (n.d.). Regular Article Nutritional Composition of Some Wild Plant …. Retrieved November 5, 2020, from https://www.sciencedirect.com/science/article/abs/pii/S0889157500909608
- (n.d.). The Paleoanthropology and Archaeology of Big … – Springer. Retrieved November 5, 2020, from https://www.springer.com/gp/book/9781441967329
- (n.d.). Animal foods in traditional Australian aboriginal diets – PubMed. Retrieved November 5, 2020, from https://pubmed.ncbi.nlm.nih.gov/3796233/
- (n.d.). 2015-2020 Dietary Guidelines | health.gov. Retrieved November 5, 2020, from https://health.gov/dietaryguidelines/2015/guidelines/
- (2000, March 1). Hunter-gatherer diets—a different perspective | The American …. Retrieved November 5, 2020, from https://academic.oup.com/ajcn/article/71/3/665/4729104
- (2000, March 1). Hunter-gatherer diets—a different perspective | The American …. Retrieved November 5, 2020, from https://academic.oup.com/ajcn/article/71/3/665/4729104
- (2000, December 1). Reply to L Cordain et al | The American Journal of Clinical …. Retrieved November 5, 2020, from https://academic.oup.com/ajcn/article/72/6/1590/4729630
- (n.d.). Plant-animal subsistence ratios and macronutrient energy …. Retrieved November 5, 2020, from https://pubmed.ncbi.nlm.nih.gov/10702160/
- (2000, March 1). Hunter-gatherer diets—a different perspective | The American …. Retrieved November 5, 2020, from https://academic.oup.com/ajcn/article/71/3/665/4729104
- “Vitamin and Mineral Supplements: Do We Really Need Them?.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3309636/. Accessed 21 Oct. 2020.
- “Food Availability (Per Capita) Data System ….” https://www.ers.usda.gov/data-products/food-availability-per-capita-data-system/. Accessed 21 Oct. 2020.
- “Obesity as an independent risk factor for cardiovascular ….” https://pubmed.ncbi.nlm.nih.gov/6219830/. Accessed 21 Oct. 2020.
- “Overweight is an independent risk factor for cardiovascular ….” https://pubmed.ncbi.nlm.nih.gov/12164466/. Accessed 21 Oct. 2020.
- “Cardiovascular risk and obesity – NCBI.” 28 Aug. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6712750/. Accessed 21 Oct. 2020.
- “Why EPIDEMIOLOGY is GARBAGE! – YouTube.” 21 Feb. 2020, https://www.youtube.com/watch?v=voGZtcFEHmk. Accessed 21 Oct. 2020.
- “Why EPIDEMIOLOGY is so MISLEADING – Paul Saladino MD.” https://www.facebook.com/carnivoreMD/videos/why-epidemiology-is-so-misleading/266279844356938/. Accessed 21 Oct. 2020.
- “Polyunsaturated fatty acids for the primary and secondary ….” 18 Jul. 2018, https://pubmed.ncbi.nlm.nih.gov/30019767/. Accessed 21 Oct. 2020.
- “A systematic review of the effect of dietary saturated and ….” https://pubmed.ncbi.nlm.nih.gov/29174025/. Accessed 21 Oct. 2020.
- “Effects of a very high saturated fat diet on LDL particles in ….” 6 Feb. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5293238/. Accessed 5 Nov. 2020.
- “A systematic review of the effect of dietary saturated and ….” https://pubmed.ncbi.nlm.nih.gov/29174025/. Accessed 5 Nov. 2020.
- “Polyunsaturated fatty acids and their effects on cardiovascular ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2719153/. Accessed 5 Nov. 2020.
- “Dietary intake and biomarkers of linoleic acid and mortality ….” 1 Jul. 2020, https://pubmed.ncbi.nlm.nih.gov/32020162/. Accessed 21 Oct. 2020.
- “Dietary linoleic acid and risk of coronary heart … – PubMed.” 28 Oct. 2014, https://pubmed.ncbi.nlm.nih.gov/25161045/. Accessed 21 Oct. 2020
- “How Linoleic Acid is making you fat and Stearic Acid might ….” 14 Sep. 2020, https://carnivoremd.com/how-linoleic-acid-is-making-you-fat-and-stearic-acid-might-just-be-the-remedy-with-brad-marshall-aka-the-croissant-diet-guy/. Accessed 21 Oct. 2020.
- “Linoleic Acid Makes You Fat and Dead Faster! Bonus mini ….” 28 Aug. 2020, https://carnivoremd.com/do-you-need-plant-fiber-for-a-healthy-gut-with-lucy-mailing-phd-2/. Accessed 21 Oct. 2020.
- “The effect of replacing saturated fat with mostly n-6 … – PubMed.” 19 May. 2017, https://pubmed.ncbi.nlm.nih.gov/28526025/. Accessed 21 Oct. 2020.
- “The effect of replacing saturated fat with mostly n-6 … – PubMed.” 19 May. 2017, https://pubmed.ncbi.nlm.nih.gov/28526025/. Accessed 21 Oct. 2020.
- “N-3 polyunsaturated fatty acids in coronary heart disease: a ….” https://pubmed.ncbi.nlm.nih.gov/11893369. Accessed 21 Oct. 2020.
- “LIFE-CVD: A New Lifetime Risk Score Model That Estimates ….” 24 Jun. 2019, https://www.acc.org/latest-in-cardiology/articles/2019/06/24/14/13/life-cvd-a-new-lifetime-risk-score-model-that-estimates-treatment-benefit. Accessed 21 Oct. 2020.
- “The effect of replacing saturated fat with mostly n … – NCBI – NIH.” 19 May. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5437600/. Accessed 21 Oct. 2020.
- “Dietary total fat, fatty acids intake, and risk of … – NCBI.” 6 Apr. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6451787/. Accessed 23 Oct. 2020.
- “Association between Plasma N-6 Polyunsaturated Fatty Acids ….” 17 Dec. 2019, https://www.nature.com/articles/s41598-019-55686-7. Accessed 23 Oct. 2020.
- “Are Excess OMEGA-6 FA Causing CANCER? – YouTube.” 8 Mar. 2020, https://www.youtube.com/watch?v=9pC5U6fow1w. Accessed 23 Oct. 2020
- “Transfer of low density lipoprotein into the arterial wall and risk ….” https://pubmed.ncbi.nlm.nih.gov/8782833/. Accessed 23 Oct. 2020.
- “Lipoprotein oxidation in cardiovascular disease: chief culprit ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2118281/. Accessed 23 Oct. 2020.
- “High LDL in the setting of metabolic… – Paul Saladino MD.” https://www.facebook.com/carnivoreMD/videos/high-ldl-in-the-setting-of-metabolic-health-indicated-by-hdl-low-trig-low-fastin/2142852902477904/. Accessed 23 Oct. 2020
- “Association between circulating oxidized low-density … – NCBI.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5627698/. Accessed 23 Oct. 2020.
- “Association Between Lowering LDL-C and Cardiovascular ….” 27 Sep. 2016, https://jamanetwork.com/journals/jama/fullarticle/2556125. Accessed 23 Oct. 2020.
- “Low-density lipoproteins cause atherosclerotic cardiovascular ….” 24 Apr. 2017, https://academic.oup.com/eurheartj/article/38/32/2459/3745109. Accessed 23 Oct. 2020.
- “Mendelian randomization: Its impact on cardiovascular disease.” 22 May. 2018, https://pubmed.ncbi.nlm.nih.gov/29801689/. Accessed 23 Oct. 2020
- “Mendelian randomization studies: using naturally randomized ….” https://pubmed.ncbi.nlm.nih.gov/26780009/. Accessed 23 Oct. 2020.
- “Mendelian randomization to assess causal effects of blood ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4816855/. Accessed 23 Oct. 2020.
- “Mendelian randomization of blood lipids for coronary heart ….” https://pubmed.ncbi.nlm.nih.gov/24474739/. Accessed 23 Oct. 2020.
- “Using Mendelian Randomization studies to Assess Causality ….” 10 Sep. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5658043/. Accessed 23 Oct. 2020.
- “Genetically-predicted life-long lowering of low-density ….” 9 Jul. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6642403/. Accessed 23 Oct. 2020.
- “Mendelian randomization studies: using naturally randomized ….” https://pubmed.ncbi.nlm.nih.gov/26780009/. Accessed 23 Oct. 2020.
- “Lowering LDL cholesterol reduces cardiovascular … – PubMed.” 14 Nov. 2017, https://pubmed.ncbi.nlm.nih.gov/29146277/. Accessed 23 Oct. 2020.
- “Is Isolated Low HDL-C a CVD Risk Factor?: New Insights from ….” 10 May. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4871717/. Accessed 28 Oct. 2020
- “Plasma HDL cholesterol and risk of myocardial infarction – NCBI.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3419820/. Accessed 23 Oct. 2020.
- “Effect of HDL-Raising Drugs on Cardiovascular Outcomes: A ….” 11 Apr. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3984171/. Accessed 23 Oct. 2020.
- “Saturated fat, especially long chain… – Paul Saladino MD ….” 20 Jun. 2020, https://www.facebook.com/carnivoreMD/posts/2897774587016466. Accessed 23 Oct. 2020.
- “Explaining the increased mortality in type 1 diabetes – NCBI.” 10 Jul. 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499523/. Accessed 28 Oct. 2020.
- “Ammonia toxicity and its prevention in inherited defects of the ….” https://pubmed.ncbi.nlm.nih.gov/19531057/. Accessed 28 Oct. 2020.
- “Macronutrient metabolism by the human gut microbiome – NCBI.” 13 Jun. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6567490/. Accessed 28 Oct. 2020.
- “LDL cholesterol still a problem in old age? A … – PubMed.” 7 Apr. 2015, https://pubmed.ncbi.nlm.nih.gov/25855712/. Accessed 28 Oct. 2020.
- “A receptor-mediated pathway for cholesterol homeostasis.” https://pubmed.ncbi.nlm.nih.gov/3513311/. Accessed 29 Oct. 2020.
- “Reduction in C-reactive protein and LDL cholesterol … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/19329177/. Accessed 28 Oct. 2020.
- “[Lipid profile in healthy newborn infants and its correlation with ….” https://pubmed.ncbi.nlm.nih.gov/11142836/. Accessed 28 Oct. 2020.
- “Management of elevated low density lipoprotein-cholesterol ….” 15 Jul. 2020, https://www.uptodate.com/contents/management-of-elevated-low-density-lipoprotein-cholesterol-ldl-c-in-primary-prevention-of-cardiovascular-disease. Accessed 28 Oct. 2020.
- “LDL Receptor Knock-Out Mice Are a … – NCBI – NIH.” 25 Jan. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3266276/. Accessed 28 Oct. 2020.
- “Atherogenesis and metabolic dysregulation in LDL receptor ….” 4 May. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5414561/. Accessed 28 Oct. 2020.
- “Characterization of atherosclerosis in LDL receptor knockout ….” https://pubmed.ncbi.nlm.nih.gov/10729382/. Accessed 28 Oct. 2020.
- “LDL receptor knock-out mice show impaired … – NCBI – NIH.” 20 Nov. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4258039/. Accessed 28 Oct. 2020.
- “Causal Inference for Genetically Determined Levels of High ….” 7 Nov. 2019, https://www.ahajournals.org/doi/10.1161/ATVBAHA.119.313381. Accessed 28 Oct. 2020.
- “High-density lipoprotein (HDL) functionality and its relevance ….” 28 Mar. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5877920/. Accessed 28 Oct. 2020.
- “High density lipoprotein and metabolic disease: Potential ….” 18 Mar. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4837296/. Accessed 28 Oct. 2020
- “Effect of HDL-Raising Drugs on Cardiovascular Outcomes: A ….” 11 Apr. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3984171/. Accessed 28 Oct. 2020
- “Plasma HDL cholesterol and risk of myocardial infarction – NCBI.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3419820/. Accessed 28 Oct. 2020.
- “Is Isolated Low HDL-C a CVD Risk Factor?: New Insights from ….” 10 May. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4871717/. Accessed 28 Oct. 2020.
- “Insulin resistance and cardiovascular disease – NCBI.” 15 Aug. 2000, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC380256/. Accessed 28 Oct. 2020.
- “Association between insulin resistance and the development ….” 31 Aug. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6119242/. Accessed 28 Oct. 2020.
- “LDL-C plays a causal role on T2DM: a Mendelian … – NCBI.” 10 Feb. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7041740/. Accessed 28 Oct. 2020.
- “HDL Cholesterol and Risk of Type 2 Diabetes: A Mendelian ….” https://diabetes.diabetesjournals.org/content/diabetes/64/9/3328.full-text.pdf. Accessed 28 Oct. 2020.
- “Impact of low-density lipoprotein cholesterol on cardiovascular ….” 9 Aug. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4141536/. Accessed 28 Oct. 2020
- “LDL Cholesterol as a Strong Predictor of Coronary Heart ….” https://www.ahajournals.org/doi/10.1161/01.ATV.20.3.830 Accessed 28 Oct. 2020.
- “Is Isolated Low HDL-C a CVD Risk Factor?: New Insights from ….” 10 May. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4871717/. Accessed 28 Oct. 2020.
- “Lowering LDL cholesterol reduces cardiovascular risk ….” 14 Nov. 2017, https://pubmed.ncbi.nlm.nih.gov/29146277/. Accessed 28 Oct. 2020.
- “Factors affecting the severity of motor vehicle traffic crashes ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1067816/. Accessed 28 Oct. 2020.
- “Fasting increases serum total cholesterol, LDL cholesterol and ….” https://pubmed.ncbi.nlm.nih.gov/10539776/. Accessed 28 Oct. 2020.
- “Hypercholesterolaemia of prolonged fasting and cholesterol ….” https://pubmed.ncbi.nlm.nih.gov/7569738/. Accessed 28 Oct. 2020.
- “Effects on cardiovascular risk factors of weight losses limited ….” 4 Nov. 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4987606/. Accessed 28 Oct. 2020
- “Atherosclerosis – NCBI – NIH.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2826222/. Accessed 28 Oct. 2020.
- “Artery interposed to vein did not develop atherosclerosis and ….” https://pubmed.ncbi.nlm.nih.gov/15488863/. Accessed 28 Oct. 2020.
- “Mendelian randomization studies: using naturally randomized ….” https://pubmed.ncbi.nlm.nih.gov/26780009/. Accessed 28 Oct. 2020
- “Mendelian randomization to assess causal effects of … – NCBI.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4816855/. Accessed 28 Oct. 2020.
- “Variable Effects Of LDL Subclasses Of Cholesterol On … – NCBI.” 18 Nov. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6874513/. Accessed 29 Oct. 2020.
- “Endothelial Transcytosis of Lipoproteins in … – NCBI.” 25 Sep. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6167422/. Accessed 29 Oct. 2020.
- “Transfer of low density lipoprotein into the arterial … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/8782833/. Accessed 29 Oct. 2020.
- “Changes in LDL Oxidative Status and Oxidative and … – NCBI.” 25 May. 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458536/. Accessed 29 Oct. 2020.
- “The Dynamics of Oxidized LDL during Atherogenesis – NCBI.” 11 May. 2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108093/. Accessed 29 Oct. 2020.
- “Short-Term Bixin Supplementation of Healthy Subjects … – NCBI.” 3 Mar. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6421732/. Accessed 29 Oct. 2020.
- “Oxidized LDL and the metabolic syndrome – NCBI – NIH.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2631666/. Accessed 29 Oct. 2020.
- “Targeting oxidized LDL improves insulin sensitivity and … – NCBI.” 11 Jun. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3773831/. Accessed 29 Oct. 2020.
- “Influence of long-chain polyunsaturated fatty acids … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/9774178/. Accessed 29 Oct. 2020.
- “Dietary Linoleic Acid and Risk of Coronary Heart Disease: A ….” 26 Aug. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4334131/. Accessed 29 Oct. 2020.
- “α-Linolenic acid and risk of cardiovascular disease: a ….” 17 Oct. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3497923/. Accessed 29 Oct. 2020.
- “The Evidence for α-Linolenic Acid and Cardiovascular … – NCBI.” 3 Nov. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4224228/. Accessed 29 Oct. 2020.
- “Alpha-linolenic acid and cardiovascular diseases – PubMed.” https://pubmed.ncbi.nlm.nih.gov/11458289/. Accessed 29 Oct. 2020.
- “The Effects of Linoleic Acid Consumption on Lipid Risk ….” 4 Aug. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7469037/. Accessed 29 Oct. 2020.
- “Linoleic acid-rich fats reduce atherosclerosis development ….” https://pubmed.ncbi.nlm.nih.gov/16351765/. Accessed 29 Oct. 2020.
- “Test of effect of lipid lowering by diet on … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/2643423/. Accessed 29 Oct. 2020.
- “Mendelian randomization: Its impact on cardiovascular disease.” 22 May. 2018, https://pubmed.ncbi.nlm.nih.gov/29801689/. Accessed 29 Oct. 2020.
- “Mendelian randomization to assess causal effects of blood ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4816855/. Accessed 29 Oct. 2020.
- “Evaluating the relationship between circulating lipoprotein ….” 23 Mar. 2020, https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003062. Accessed 29 Oct. 2020.
- “Test of effect of lipid lowering by diet on … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/2643423/. Accessed 29 Oct. 2020.
- “Helsinki Heart Study: primary-prevention trial with gemfibrozil ….” 12 Nov. 1987, https://pubmed.ncbi.nlm.nih.gov/3313041/. Accessed 29 Oct. 2020.
- “Ezetimibe Added to Statin Therapy after Acute Coronary ….” 18 Jun. 2015, https://pubmed.ncbi.nlm.nih.gov/26039521/. Accessed 30 Oct. 2020.
- “Effect of long-term exposure to lower low-density … – PubMed.” 25 Dec. 2012, https://pubmed.ncbi.nlm.nih.gov/23083789/. Accessed 30 Oct. 2020.
- “Effect of long-term exposure to lower low-density … – PubMed.” 25 Dec. 2012, https://pubmed.ncbi.nlm.nih.gov/23083789/. Accessed 30 Oct. 2020.
- “Polyunsaturated fatty acids for the primary and secondary ….” 18 Jul. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6513571/. Accessed 30 Oct. 2020.
- “Effect of the amount and type of dietary fat on cardiometabolic ….” 10 Jul. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4095759/. Accessed 30 Oct. 2020.
- “Effect of dietary fiber on constipation: A meta analysis.” 28 Dec. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3544045/. Accessed 30 Oct. 2020.
- “Systematic review with meta-analysis: effect of fibre … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/27170558/. Accessed 30 Oct. 2020.
- “Systematic review: the effects of fibre in the … – PubMed.” 20 Feb. 2011, https://pubmed.ncbi.nlm.nih.gov/21332763/. Accessed 2 Nov. 2020.
- “Stopping or reducing dietary fiber intake reduces constipation ….” 7 Sep. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435786/. Accessed 30 Oct. 2020.
- “Systematic review with meta-analysis of the … – BMC Cancer.” 3 Sep. 2012, https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-12-385. Accessed 2 Nov. 2020.
- “Dietary fibre intake and mortality from cardiovascular disease ….” https://pubmed.ncbi.nlm.nih.gov/26711548/. Accessed 3 Nov. 2020
- “Dietary Fiber Is Beneficial for the Prevention of … – NCBI – NIH.” 25 Oct. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5731843/. Accessed 3 Nov. 2020.
- “Association between dietary fiber intake and risk of coronary ….” https://pubmed.ncbi.nlm.nih.gov/24929874/. Accessed 3 Nov. 2020.
- “Dietary fiber intake and risk of cardiovascular disease ….” 19 Dec. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3898422/. Accessed 3 Nov. 2020.
- “Dietary Fiber, Atherosclerosis, and Cardiovascular Disease.” 23 May. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6566984/. Accessed 3 Nov. 2020.
- “Dietary Fiber Is Beneficial for the Prevention of … – NCBI – NIH.” 25 Oct. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5731843/. Accessed 3 Nov. 2020.
- “The Benefits of Dietary Fiber Intake on Reducing the Risk of ….” 14 Jun. 2018, https://pubmed.ncbi.nlm.nih.gov/30166965/. Accessed 3 Nov. 2020
- “Association between dietary fiber intake and risk of ovarian ….” 24 Aug. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166337/. Accessed 3 Nov. 2020
- “Rectal Cancer: 20% Risk Reduction Thanks to Dietary Fibre ….” 12 Jul. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6683071/. Accessed 3 Nov. 2020.
- “Meat consumption and cancer risk: a critical review of ….” https://pubmed.ncbi.nlm.nih.gov/26633248/. Accessed 3 Nov. 2020.
- “Red and Processed Meat and Mortality in a Low Meat Intake ….” 14 Mar. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6470727/. Accessed 3 Nov. 2020.
- “Animal and plant protein intake and all-cause and cause ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5048552/. Accessed 3 Nov. 2020
- “Co-consumption of Vegetables and Fruit, Whole … – NCBI – NIH.” 29 Jul. 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7468967/. Accessed 3 Nov. 2020.
- “Ancestors’ dietary patterns and environments could drive ….” 4 Oct. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5628472/. Accessed 2 Nov. 2020
- “Diet and the evolution of the earliest human ancestors – NCBI.” 28 Nov. 2000, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC17605/. Accessed 2 Nov. 2020.
- “Comparative Digestive Physiology – NCBI – NIH.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4458075/. Accessed 2 Nov. 2020.
- “Cats and Carbohydrates: The Carnivore Fantasy? – NCBI – NIH.” 15 Nov. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5753635/. Accessed 2 Nov. 2020.
- “Diet of chimpanzees (Pan troglodytes schweinfurthii … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/22109938/. Accessed 2 Nov. 2020.
- “Hunter-Gatherer Energetics and Human Obesity – NCBI – NIH.” 25 Jul. 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405064/. Accessed 2 Nov. 2020.
- “Hunter-gatherers as models in public health – PubMed.” https://pubmed.ncbi.nlm.nih.gov/30511505/. Accessed 2 Nov. 2020.
- “Optimal low-density lipoprotein is 50 to 70 mg/dl | JACC ….” 2 Jun. 2004, https://www.onlinejacc.org/content/43/11/2142. Accessed 2 Nov. 2020.
- “Physical activity patterns and biomarkers of cardiovascular ….” 9 Oct. 2016, https://pubmed.ncbi.nlm.nih.gov/27723159/. Accessed 2 Nov. 2020.
- “Physical activity patterns and biomarkers of cardiovascular ….” 9 Oct. 2016, https://pubmed.ncbi.nlm.nih.gov/27723159/. Accessed 2 Nov. 2020.
- “Physical activity patterns and biomarkers of cardiovascular ….” 9 Oct. 2016, https://pubmed.ncbi.nlm.nih.gov/27723159/. Accessed 2 Nov. 2020.
- “Lipoprotein profiles in Alaskan Siberian Yupik Eskimos.” https://pubmed.ncbi.nlm.nih.gov/9115542/. Accessed 2 Nov. 2020.
- “Lipoprotein profile of a Greenland Inuit population. Influence ….” https://pubmed.ncbi.nlm.nih.gov/1450169/. Accessed 2 Nov. 2020.
- “Low incidence of cardiovascular disease among the Inuit ….” https://pubmed.ncbi.nlm.nih.gov/12535749/. Accessed 2 Nov. 2020.
- “Cardiovascular burden and related risk factors among ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2903990/. Accessed 2 Nov. 2020.
- “Cardiovascular Disease Prevalence and its Relation to Risk ….” 2 Oct. 2009, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2981096/. Accessed 2 Nov. 2020.
- “Fishing” for the origins of the “Eskimos and heart disease ….” https://pubmed.ncbi.nlm.nih.gov/25064579/. Accessed 2 Nov. 2020.
- “Impact of grass/forage feeding versus grain finishing on beef ….” https://pubmed.ncbi.nlm.nih.gov/24018274/. Accessed 3 Nov. 2020.
- “Systematic review and meta-analysis of glyphosate exposure ….” 25 Mar. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4866614/. Accessed 3 Nov. 2020.
- “A Meta-Analysis to Estimate the Placebo Effect in Randomized ….” https://pubmed.ncbi.nlm.nih.gov/26749157/. Accessed 3 Nov. 2020.
- “A systematic review and meta-analysis of placebo versus no ….” https://pubmed.ncbi.nlm.nih.gov/28554719/. Accessed 3 Nov. 2020
- “Meta-analysis of pain and function placebo responses in ….” 15 Jul. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6631867/. Accessed 3 Nov. 2020
- “Are Treatments More Effective than Placebos? A Systematic ….” 15 May. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3655171/. Accessed 3 Nov. 2020.
- “The neuroscience of placebo effects: connecting context ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6013051/. Accessed 3 Nov. 2020
- “How Placebos Change the Patient’s Brain – NCBI – NIH.” 30 Jun. 2010, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3055515/. Accessed 3 Nov. 2020.
- “Placebo effects and the molecular biological components ….” 6 Sep. 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6738668/. Accessed 3 Nov. 2020
- “The concentration of creatine in meat, offal and … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/9160426/. Accessed 3 Nov. 2020
- “Effects of creatine and creatinine content on the … – PubMed.” https://pubmed.ncbi.nlm.nih.gov/3679021/. Accessed 3 Nov. 2020.