Recently, I wrote an article titled, The Impact of Exercise on the Male Sex Life for Biolayne and you all loved it. Naturally, I had to do a follow up with how exercise impacts the female sex life. I hope you all enjoy.
Humans are complex. Women in particular are more complicated because there is a lack of research out there in comparison to all the research done for and on men. Researchers study the hell out of erectile dysfunction, but for women, sexual dysfunction isn’t as visible as erectile dysfunction and there’s no real equivalent, which makes the subject more complicated. Nevertheless, women do experience low sex drive which has the potential to greatly impact quality of life.
Approximately 58% of women in the United States report having impaired sexual function, which includes low sexual desire and/or arousal, difficulty reaching orgasm, and the presence of sexual pain. [1] Surprisingly, the prevalence of impaired sexual function is higher than that of depression and social anxiety. [1] What’s worse is that people with sexual dysfunction may be unknowingly making the situation worse. Barlow’s model of sexual dysfunction states that individuals with sexual dysfunction often enter into sexual situations with negative expectations and their attentional focus is typically drawn to non-erotic stimuli such as external stressors, body image concerns, and the consequences of perceived poor sexual performance. Barlow’s model of sexual dysfunction also states that focusing on non-erotic stimuli during sexual activity may increase anxiety and maintain low levels of arousal which may create a cycle of continued poor performance and later avoidance of erotic cues and sexual situations. Avoidance has been identified as a key factor in maintaining the dysfunctional sexual cycle by preventing new learning which could change the sexual experience and therefore change the mindset of the individual going forward. [1]
In fact, a team of researchers studied the dysfunctional sexual cycle mentioned above, to explore the negative consequences of impaired sexual function that may continue personal distress regarding sexual activity in women. The 87 women who participated had a mean age of 27.4 years, were mostly white, and 28% reported being married while the rest reported being in a monogamous heterosexual romantic relationship. Participants in the study agreed to attempt to engage in sexual intercourse with their partner at least five times over the course of four weeks. After each sexual experience, participants assessed their experience based on specific items using the Measure of Sexual Consequences which assessed the frequency of various potential negative consequences of impaired sexual function. The results of the study showed decreased physical pleasure during sexual activity resulted in reduced frequency of sexual activity and decreased their partner’s pleasure. [1]
This shouldn’t be surprising to anyone considering one of the main motives for engaging in sexual activity is physical pleasure, and if it doesn’t feel good, why do it again? As stated in Barlow’s model of sexual dysfunction, avoidance is a key factor in maintaining the dysfunctional sexual cycle. If the sexual experience is less than desirable, a future sexual encounter is less likely and the negative learning continues making it more difficult to create new, pleasurable sexual experiences.
This is an important starting point because sexual satisfaction has been shown to be a key component to general wellness among middle-aged women even to the extent that increased levels of sexual activity have been related to improved physical and mental health. Not to mention, sexual pleasure has been associated with enhanced marital relationships. [2]
Some other contributing factors to sexual dysfunction worth noting include but, are not limited to:
- Loss of vigor and youth/increased age [2]
- Changes in family structure [2]
- Inability to become pregnant [2]
- Loss of a sexual partner [2]
- Guilt or embarrassment over sexual desire [2]
- Marital difficulties [2]
- Drugs that may interfere with libido or performance [2]
What can women do to have better sex?
A study [2] measured 360 healthy women aged 40-65 years old to assess the determinants of sexual dysfunction among middle-aged Brazilian women. The study used the Female Sexual Function Index (FSFI) to evaluate sexual function. The FSFI is widely used and has previously been validated. Researchers also used the International Physical Activity Questionnaire (IPAQ) to determine the level of physical activity of participants. The main findings of the study were as follows:
- 67% of participants reported sexual dysfunction.
- Women with strong menopausal symptoms were 21.7 times more likely to exhibit sexual dysfunction compared with asymptomatic women.
- Women considered to have a low quality of life were 6.6 times more likely to be sexually dysfunctional compared with those classified as having a high quality of life.
- The highest prevalence of sexual dysfunction were women aged 56-65 years
- Physical activity level was found to influence sexuality among middle-aged women. 78.9% of “sedentary” women reported sexual dysfunction while only 57.6% of women classified as “very active” reported sexual dysfunction.
Another study [3] conducted on 52 women (29 premenopausal; 23 menopausal) and 66 age and menopausal status matched women (37 premenopausal; 29 menopausal) to investigate the relationship between the amount and distribution of body fat and sexual function with control, age matched women. Again, the researchers used the FSFI to determine sexual function of the participants. FSFI strongly correlated with BMI in women with FSD. When observing the data, the FSFI can be broken down into six domains: desire, pain, arousal, lubrication, orgasm, and satisfaction. Interestingly, desire and pain did not correlate with BMI however, there was a strong and inverse correlation between BMI, arousal, lubrication, orgasm, and satisfaction.
To me, these studies indicates there is a potential relationship between increased body size, body image and self confidence with sexual satisfaction because there is no correlation between desire and BMI however, BMI was inversely related to all of the exciting parts of sex like arousal, lubrication, orgasm, and satisfaction. Let’s check out one more study to see if this theory holds true.
A study [4] conducted on 45 otherwise healthy obese and overweight women and 30 control subjects with a normal BMI, assessed the frequency of female sexual dysfunction (FSD) among obese and overweight women. Again, they used the FSFI to determine female sexual function. While there was no correlation between FSFI scores and body mass index, waist-hip ratio, and body fat percentage, there was a significant correlation between BMI and orgasm; sexual satisfaction was also negatively correlated with weight.
Again, we see BMI and sexual functioning had no relationship however, the pleasurable aspects of sex suffered as BMI increased.
What does all of this mean?
First, it says that a lot of women are probably not having as good of sex as they could be, which is problematic because improvements in sexual satisfaction and sexual functioning may also improve overall quality of life. [5] And although there is some conflicting data, there could potentially be a relationship between BMI and at least certain categories of the FSFI such as arousal, lubrication, and satisfaction, all of which could play a large part in a sexual experience being a pleasurable experience or not. If the experience is not pleasurable, it is certainly conceivable to see how Barlow’s model of sexual dysfunction could be a self-fulfilling prophecy. Especially considering women who have poorer body image are more likely to report problems of sexual functioning than those who do not. [6]
Also we should note that women with menopausal symptoms were much more likely to experience sexual dysfunction compared to asymptomatic women and women who experience menopausal symptoms are more likely to be 50 years or older. And although aging typically comes with the prospect of less sex and reduced sexual functioning, there may be some good news related for those of us who are aging – physical activity may influence sexuality and reduce sexual dysfunction.
A study [7] of a 50+ Fitness Association, an organization for older people who are bonded by the pursuit of a physically active lifestyle, has data to show that as a woman, the more fit you are, the more sex you have. 30%, 38%, and 66% of the females who reported one or more bouts of sexual intimacy per week were the least, middle, and most fit groups, respectively. Meaning, the most fit group was having more than double the sexual intimacy compared to the least fit group.
And just in case you thought exercise might only benefit an aging population when it comes to sexual dysfunction, I have one more interesting study to check out.. Especially because of the detail the researchers examined their questions. A study [8] examined self-reported exercise and sexual performance data from a sample of 509 participants who were considered generally healthy adults ranging in age from 18-74 years old. Researchers used a 30-item survey which asked questions regarding exercise behavior and sexual performance. The researchers examined their hypotheses by asking specific questions relating to exercise types, frequency, duration and intensity as well as specific sexual functioning questions such as:
- “How often do you have adequate vaginal lubrication for sexual activity?”
- “How often do you desire to engage in sexual activity?”
- “How often do you become sexually aroused?”
- “How often are you easily aroused?”
- “How often do you become aroused and then lose interest?”
- “Are you able to have an orgasm when you want to?”
The results are just as interesting. The study [8] found that intensity of exercise significantly explained frequency of sexual arousal, frequency of sexual desire, frequency of sexual intercourse, and orgasms in a single sexual episode. And if that’s not enough, frequency of exercise significantly impacted frequency of sexual desire. To be specific, here are some of the findings:
| Exercise Type | Sexual Function | Odds Ratio | Meaning |
|---|---|---|---|
| RPE of Aerobics | Frequency of Sexual Arousal | 3.15 | participants who reported higher RPE during aerobics were over three times more likely to report higher frequency of sexual arousal compared to those who reported lover RPE during aerobics |
| RPE of Aerobics | Frequency of Sexual Intercourse | 2.80 | participants who reported higher RPE during aerobics were almost three times more likely to report higher frequency of sexual intercourse compared to those who reported lower RPE during aerobics |
| RPE of Strength Training | Frequency of Sexual Desire | 3.25 | participants who reported higher RPE during strength training were over three times more likely to report higher frequency of sexual desire compared to those who reported lover RPE during strength training |
| *Recreation Frequency | Frequency of Sexual Desire | 7.12 | participants who reported higher recreation frequency were over seven times more likely to report higher frequency of sexual desire compared to those who reported lower recreation frequency |
| Aerobic Frequency | Frequency of Sexual Desire | 5.60 | participants who reported higher aerobic frequency were over five times more likely to report higher frequency of sexual desire compared to those who reported lower exercise frequency |
* Recreation activities from the study included hiking, canoeing, and wilderness trips.
It’s worth noting that high blood pressure, as you may remember from the The Impact of Exercise on the Male Sex Life, had a negative impact on sexual performance, which is true for both males and females. As shown in this study, exercise frequency and intensity can have a positive impact on frequency of sexual desire and intercourse. The authors briefly mention the potential relationship between sexual desire and intercourse and exercise could be due to the impact exercise has on hypertension. Exercise helps to normalize blood pressure which increases blood flow to the genital region, which is especially important in the ability to orgasm. Another mechanism noted by the researchers related to the positive impact exercise had on sexual desire and intercourse was the impact exercise may have in increasing testosterone levels.
As a woman, which I am not, you may have already known that lower levels of estrogen and progesterone can cause vaginal dryness, hot flashes, night sweats, painful intercourse, mood swings, sleeplessness, anxiety, and depression. Not only that, lower levels of testosterone are also associated with less sexual desire. [2]
Testosterone and a Woman’s Libido
First, it appears that women with low libido may have significantly lower androgen levels compared to age-matched healthy volunteers with compared BMI and menopausal status. [9]
589 women completed a 52-week study [10] which compared three groups: placebo, 150 μg testosterone per day, and 300 μg testosterone per day delivered via a transdermal patch. The women who participated had either surgically induced menopause or were postmenopausal for at least 12 months and all participants were in a stable monogamous relationship with a sexually functional partner for at least one year prior to the study.
At baseline, approximately 50% of all sexual episodes were satisfying. At 24 weeks, the group receiving 300 μg of testosterone per day significantly increased the number of satisfying sexual episodes from baseline, an increase of 2.1 episodes per month compared to an increase of only 0.7 episodes per month in the placebo group. By week 24, 78% of sexual episodes were satisfying in the 300 μg testosterone group compared to 65% in the placebo group.
Clearly there is a large effect happening because the control group increased their satisfying sexual episodes by 65% however, the testosterone group had an additional 13% of their sexual episodes classified as satisfying which is a large enough number to affect many people’s lives. Meaning that testosterone seems have an significant impact on whether sexual episodes are pleasurable or not. The researchers agree, having found that the patch delivering 300 μg testosterone per day significantly improved sexual function and decreased distress in postmenopausal women who were not receiving estrogen therapy.
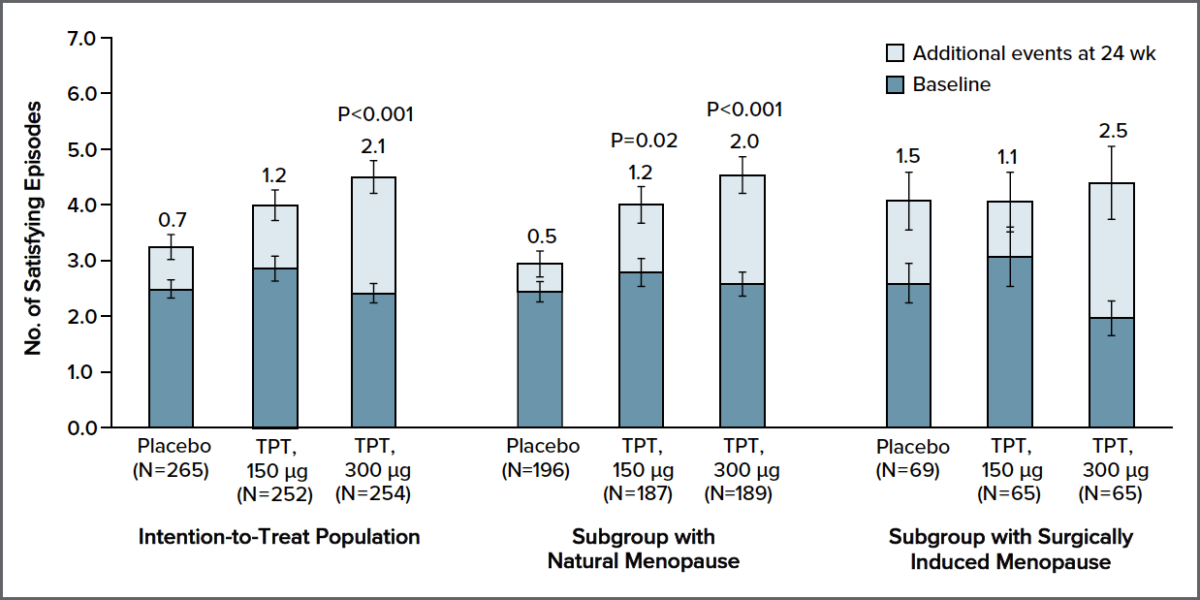
Figure: Four-Week Frequency of Satisfying Sexual Episodes at Week 24 as Compared with Baseline. P values comparing testosterone patch treatment (TPT) with placebo for the change from baseline at week 24 are based on Koch’s nonparametric analysis of covariance, adjusted for the type of menopause (natural or surgically induced). Values in parentheses are numbers of patients for whom baseline and post-baseline data were available. Values are 1% Winsorized means (±SE) for the number of satisfying episodes in a 4-week period.
Davis, S. R., Moreau, M., Kroll, R., Bouchard, C., Panay, N., Gass, M., … & Koch, H. (2008). Testosterone for low libido in postmenopausal women not taking estrogen. New England Journal of Medicine, 359(19), 2005-2017.
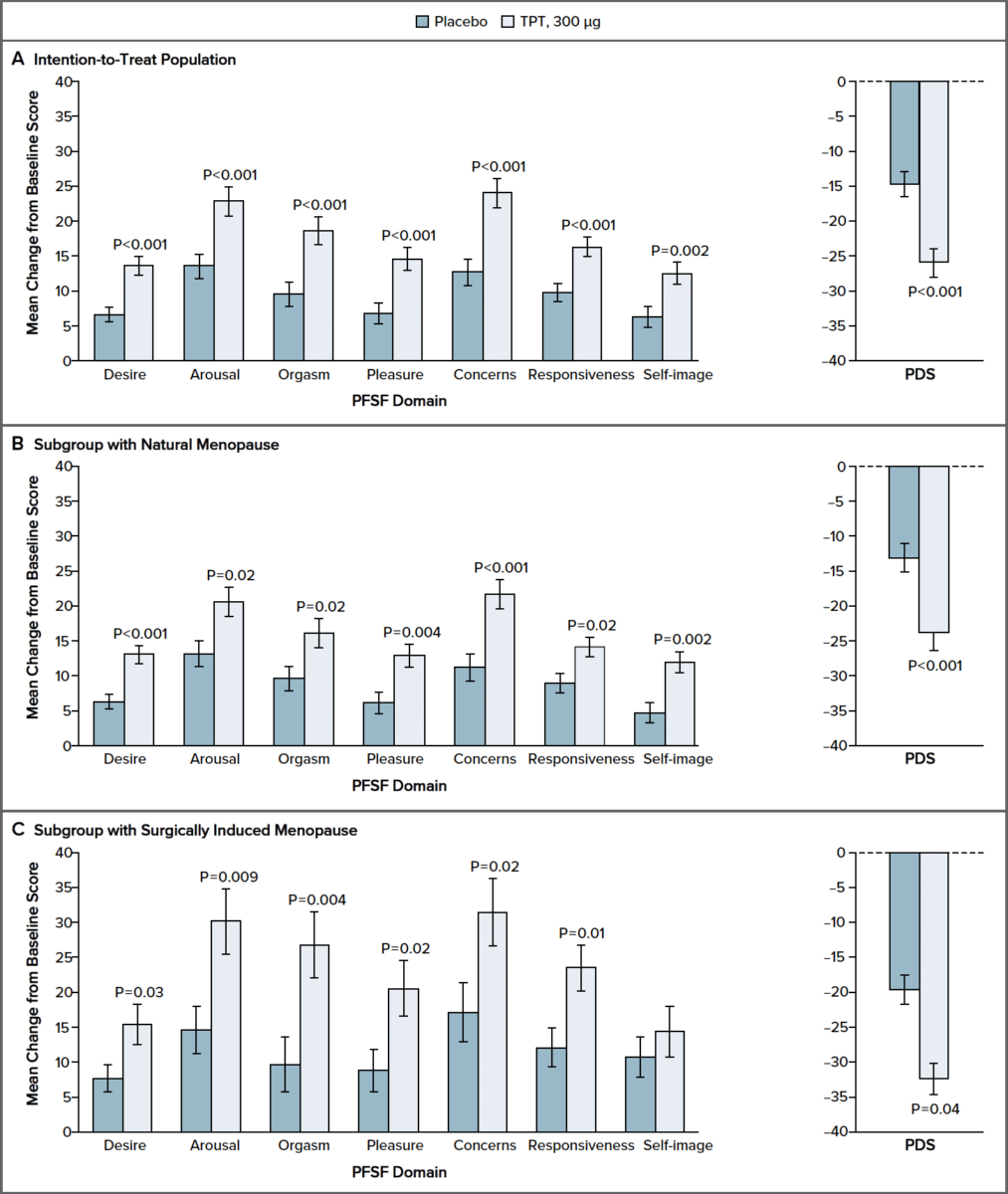
Figure: Changes from Baseline in Scores for Domains of the Profile of Female Sexual Function and for the Personal Distress Scale at Week 24.
Profile of Female Sexual Function (PFSF) domain scores
range from 0 to 100, with higher scores indicating increased sexual functioning or decreased concerns — that is, a positive change indicates improved sexual functioning and decreased sexual concerns. Personal Distress Scale (PDS) scores range from 0 to 100, with lower scores indicating less distress — that is, a negative change reflects a decrease in distress. P values for all comparisons shown are based on analysis of variance adjusted for type of menopause. In Panel C, no P value is given for self-image because the mean change in score was not significantly different from that for placebo. TPT denotes testosterone patch treatment.
Davis, S. R., Moreau, M., Kroll, R., Bouchard, C., Panay, N., Gass, M., … & Koch, H. (2008). Testosterone for low libido in postmenopausal women not taking estrogen. New England Journal of Medicine, 359(19), 2005-2017.
This is not the only study that shows a similar effect of testosterone increasing a woman’s libido.
A 24-week, double blind, placebo-controlled study recruited women aged 20-70 years old, in good health, who had undergone bilateral salpingo-oophorectomy and hysterectomy at least six months before screening to investigate the efficacy and safety of a 300 μg testosterone per day patch. [11] In addition, the women had to have reported having a satisfying sex life before oophorectomy and a meaningful loss of sexual desire and decrease in sexual activity after surgery as well as being bothered or concerned about their decrease in sexual activity and desire.
Definitions:
Oophorectomy – removal of one or both ovaries and fallopian tubes
Hysterectomy – removal of a woman’s uterus
Women who have undergone bilateral oophorectomy typically experience a drop of approximately 50% in their circulating testosterone levels. [11]
The study showed after 24-weeks the testosterone patch treatment significantly increased the frequency of total sexual episodes and orgasms. The testosterone patch treatment group also significantly improved their baseline sexual desire score, significantly decreased their personal distress, and experienced significantly more favorable changes in all other domains of the PFSF compared to the placebo group. (PFSF domains include: sexual desire, sexual pleasure, arousal, orgasm, sexual responsiveness, sexual concerns, and sexual self-image)
Clearly based on these two studies, increasing testosterone by 300 μg has had positive effects on women. But what about negative effects? Neither study showed much to be concerned about regarding androgenic events (acne, unwanted hair growth, voice deepening, etc.) due to the testosterone therapy. In fact, in one of the studies the testosterone group experienced lower rates of androgenic events compared to the placebo group [11].
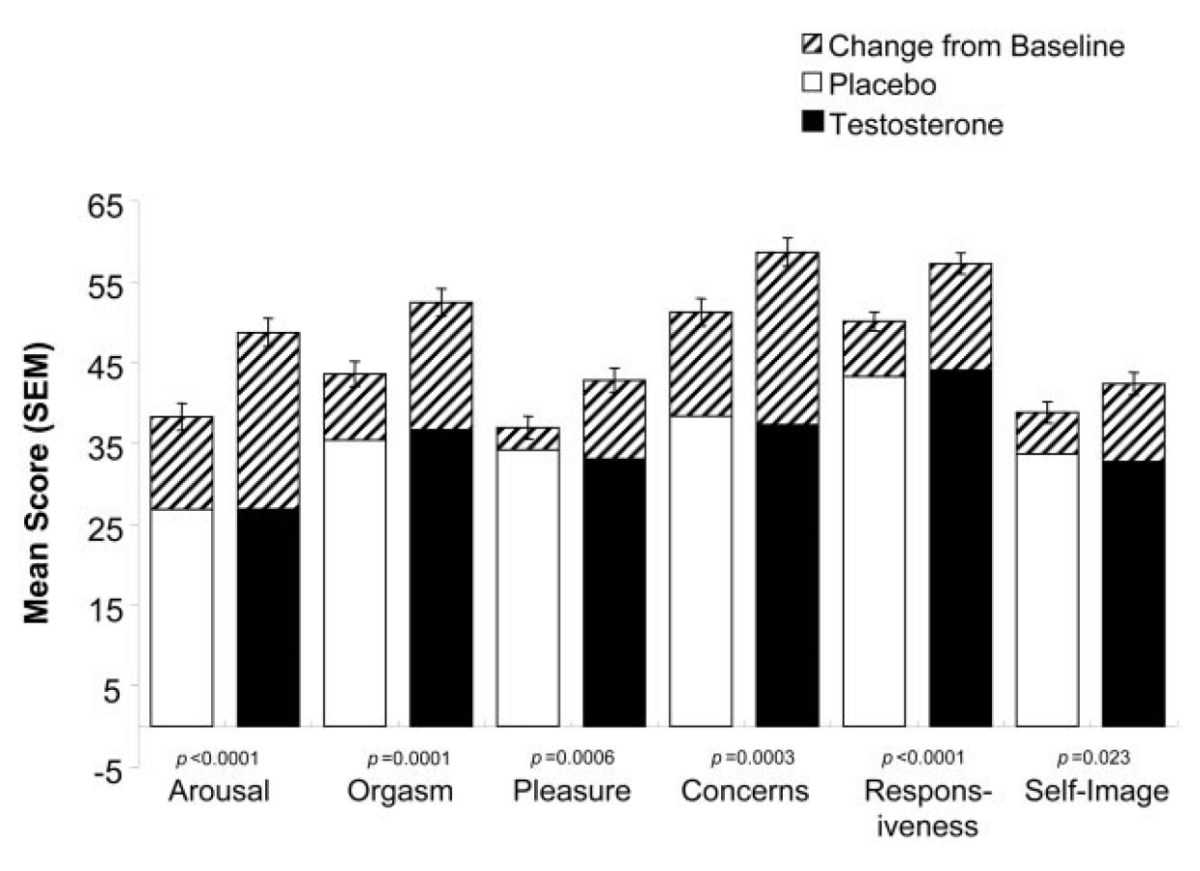
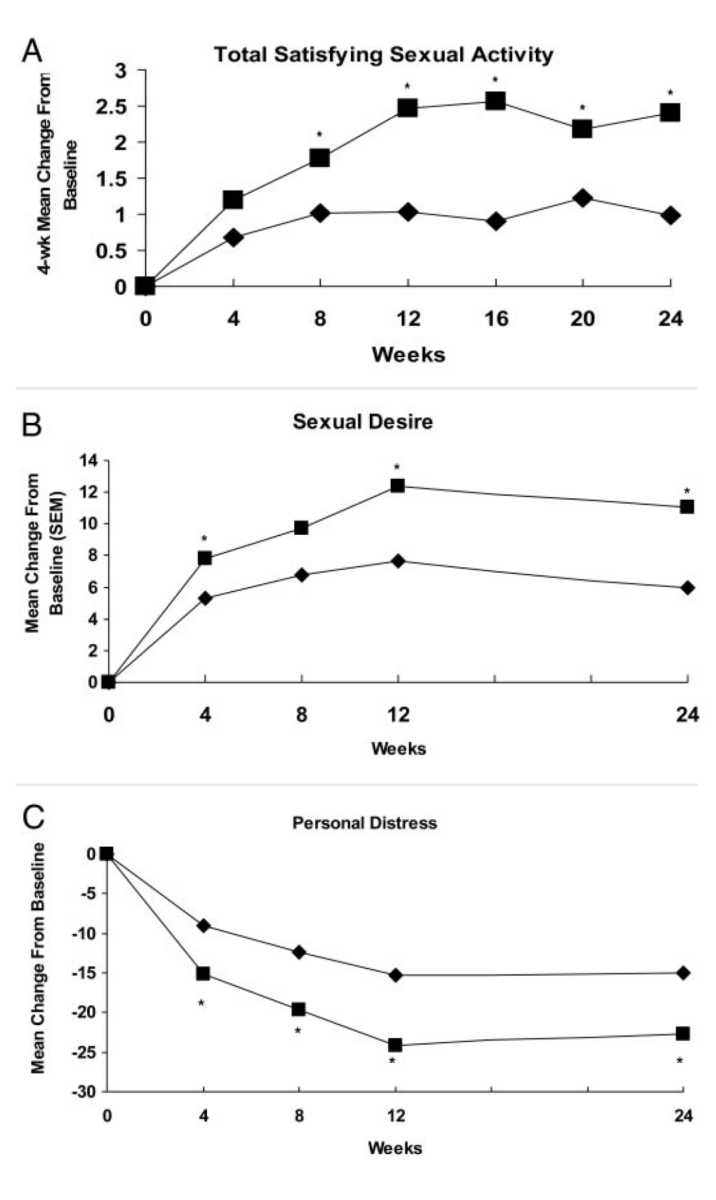
Simon, J., Braunstein, G., Nachtigall, L., Utian, W., Katz, M., Miller, S., … & Rodenberg, C. (2005). Testosterone patch increases sexual activity and desire in surgically menopausal women with hypoactive sexual desire disorder. The Journal of Clinical Endocrinology & Metabolism, 90(9), 5226-5233.
Increased testosterone does have a positive impact on sexual experiences in women but it does raise one question.
Does Exercise Increase Testosterone in Females?
A study [12] measured the effect exercise has on sexual arousal as well as how testosterone changes in relation to acute exercise. To do this, researchers recruited 16 women aged 18-45 years who had not yet reached menopause, were free of sexual problems and any drugs, medical conditions, or medications that could affect sexual arousal. The study contained two groups, exercise and non-exercise. Both groups filled out a series of questionnaires and provided a saliva sample to measure testosterone, then waited ten minutes to provide a second saliva sample. Following that, participants inserted a vaginal photoplethysmography (VPA — an instrument used to measure changes in volume, in this case blood, within an organ) and attached the ECG electrodes and, once comfortable, watched a series of films. The first being a one-minute video displaying the word “relax”, then three minutes of a neutral film such as a travel documentary, and finally a ten-minute video of a woman-centered sexual film. The only difference between the groups was the exercise group performed 20 minutes of exercise on a treadmill, 15 of which was at their target heart rate level. After the 20 minutes, participants waited ten minutes to provide their second saliva sample.
Data showed the mean percentage increase between neutral and erotic films for the no-exercise group was 31.5%, which was significant while the exercise group was 55.9%, also significant. While exercise did increase the VPA, indicating women had higher levels of genital arousal after exercise, it did not appear that testosterone was a factor. There were no changes in testosterone and no differences in testosterone between conditions.
Another study [13] compared low-volume circuit type weight training (SSC) versus periodized high-volume resistance training (MS) on 34 active but untrained, young, healthy women over the course of 24 weeks. Results of this study showed that at 24 weeks, the periodized high-volume resistance training group significantly increased resting serum testosterone concentrations compared to baseline, the low-volume group, and a control group.
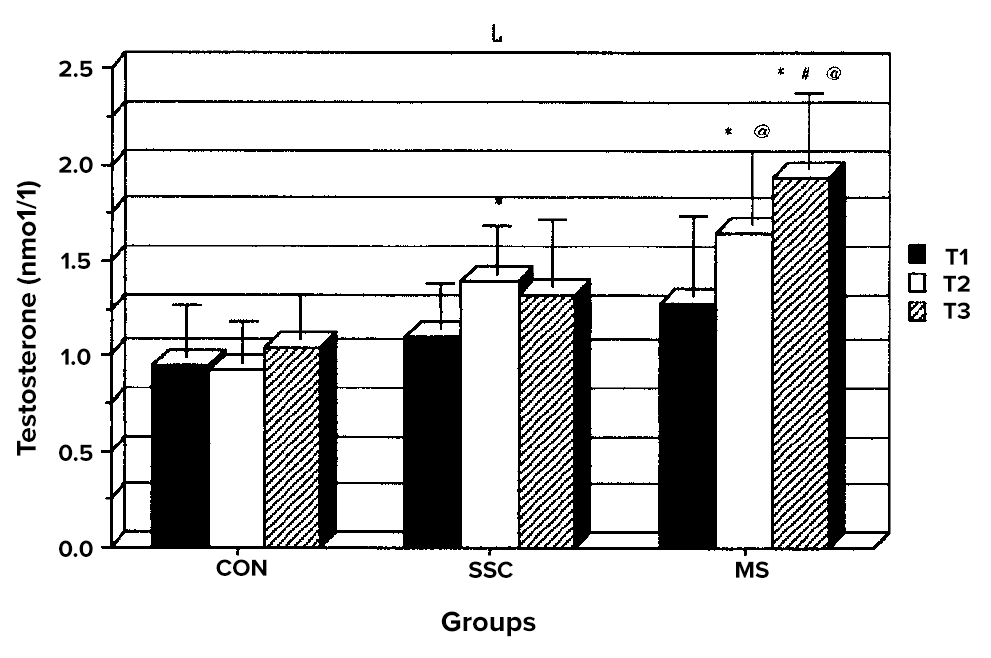
The effects of low- and high-volume resistance training on resting serum testosterone concentrations in women. * P < 0.05 from corresponding preexercise time point T1. # P < 0.05 from corresponding time point T2. @ P < 0.05 between groups.
Marx, J. O., RATAMESS, N. A., NINDL, B. C., GOTSHALK, L. A., VOLEK, J. S., Dohi, K. E. I. I. C. H. I. R. O., … & HÄKKINEN, K. (2001). Low-volume circuit versus high-volume periodized resistance training in women. Medicine & Science in Sports & Exercise, 33(4), 635-643
Based on this evidence we can see there is some data that show exercise can increase in resting serum testosterone levels compared to baseline, however, there are other studies that do not show the same increases in testosterone following exercise. [11][14][15] If there is any hope for women to increase your testosterone levels based on exercise alone, it is probably best to follow a periodized resistance training program consisting of compound movements completed over at least 6 months. But even this will not increase your testosterone as much as the transdermal patches used in the previous studies mentioned.
But that’s all still OK because even if exercise doesn’t increase testosterone in females, there is obviously still a lot to gain from exercise in the way of enhancing your sexual experiences. Let’s review the key points from the article as a recap:
Key Points
- Approximately 58% of women in the United States report having impaired sexual function, which includes low sexual desire and/or arousal, difficulty reaching orgasm, and the presence of sexual pain. [1]
- When sexual activities are not fun, people have less sex. Antidepressant medication, external stressors, body image concerns, and perceived poor sexual performance can all reduce the pleasure associated with sexual activities. When people anticipate their future sexual activities to be less than desirable, it can become a cyclical self-fulfilling prophecy based which is what Barlow’s model of sexual dysfunction states.
- Women who have low libido, specifically those women who are postmenopausal or have undergone oophorectomy or hysterectomy procedures may benefit from testosterone therapy. Check with you doctor.
- There is conflicting data related to exercises ability to increase baseline testosterone levels in women. However, even if exercise doesn’t increase a women’s testosterone levels, physical activity level was found to influence sexuality among middle-aged women.
- Intensity and frequency of exercise have shown to be important in increasing sexual arousal, sexual desire, increased sexual intercourse, and orgasm frequency in women.
- Because of the vast amount of research that has been done looking at exercise and the impact on male sexual dysfunction, there is a much clearer picture for men. More research is clearly needed to have a better understanding of how exercise impacts a woman’s sex life.
References
- Stephenson, K. R., & Meston, C. M. (2015). Why is impaired sexual function distressing to women? The primacy of pleasure in female sexual dysfunction. The journal of sexual medicine, 12(3), 728-737.
- Cabral, P. U., Canário, A. C., Spyrides, M. H., Uchôa, S. A., Eleutério Jr, J., & Gonçalves, A. K. (2013). Determinants of sexual dysfunction among middle‐aged women. International Journal of Gynecology & Obstetrics, 120(3), 271-274.
- Esposito, K., Ciotola, M., Giugliano, F., Bisogni, C., Schisano, B., Autorino, R., … & Giugliano, D. (2007). Association of body weight with sexual function in women. International journal of impotence research, 19(4), 353.
- Yaylali, G. F., Tekekoglu, S., & Akin, F. (2010). Sexual dysfunction in obese and overweight women. International journal of impotence research, 22(4), 220.
- Jiannine, L. M. (2018). An investigation of the relationship between physical fitness, self-concept, and sexual functioning. Journal of Education and Health Promotion, 7.
- Weaver, A. D., & Byers, E. S. (2006). The relationships among body image, body mass index, exercise, and sexual functioning in heterosexual women. Psychology of Women Quarterly, 30(4), 333-339.
- Bortz 2nd, W. M., & Wallace, D. H. (1999). Physical fitness, aging, and sexuality. Western Journal of Medicine, 170(3), 167.
- Morris, D., Marshall, S. A., & Demers, D. (2018). Exercise Predictors of Self-Reported Sexual Performance among Healthy Adults. International Journal of Health Sciences, 6(1), 1-16.
- Turna, B., Apaydin, E., Semerci, B., Altay, B., Cikili, N., & Nazli, O. (2005). Women with low libido: correlation of decreased androgen levels with female sexual function index. International journal of impotence research, 17(2), 148.
- Davis, S. R., Moreau, M., Kroll, R., Bouchard, C., Panay, N., Gass, M., … & Koch, H. (2008). Testosterone for low libido in postmenopausal women not taking estrogen. New England Journal of Medicine, 359(19), 2005-2017.
- Simon, J., Braunstein, G., Nachtigall, L., Utian, W., Katz, M., Miller, S., … & Rodenberg, C. (2005). Testosterone patch increases sexual activity and desire in surgically menopausal women with hypoactive sexual desire disorder. The Journal of Clinical Endocrinology & Metabolism, 90(9), 5226-5233.
- Hamilton, L. D., Fogle, E. A., & Meston, C. M. (2008). The roles of testosterone and alpha-amylase in exercise-induced sexual arousal in women. The journal of sexual medicine, 5(4), 845-853.
- Marx, J. O., RATAMESS, N. A., NINDL, B. C., GOTSHALK, L. A., VOLEK, J. S., Dohi, K. E. I. I. C. H. I. R. O., … & HÄKKINEN, K. (2001). Low-volume circuit versus high-volume periodized resistance training in women. Medicine & Science in Sports & Exercise, 33(4), 635-643.
- Linnamo, V., Pakarinen, A., Komi, P. V., Kraemer, W. J., & Häkkinen, K. (2005). Acute hormonal responses to submaximal and maximal heavy resistance and explosive exercises in men and women. Journal of strength and conditioning research, 19(3), 566.
- Kraemer, W. J., Fleck, S. J., Dziados, J. E., Harman, E. A., Marchitelli, L. J., Gordon, S. E., … & Triplett, N. T. (1993). Changes in hormonal concentrations after different heavy-resistance exercise protocols in women. Journal of applied physiology, 75(2), 594-604.





